Difference between revisions of "Germanic New Medicine"
m (→Handedness) |
|||
| (31 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
[[image:gnmen.jpg|300px|thumb]] | [[image:gnmen.jpg|300px|thumb]] | ||
[[image:Hamer2.jpg|Inventor R. G. Hamer|thumb]] | [[image:Hamer2.jpg|Inventor R. G. Hamer|thumb]] | ||
| − | '''Germanic New Medicine'''® (GNM) (formerly called ''New Medicine'' and often called ''New German[ic] Medicine'') is a pseudoscientific alternative medicine | + | '''Germanic New Medicine'''® (GNM) (formerly called ''New Medicine'' and often called ''New German[ic] Medicine'') is a pseudoscientific, alternative medicine which appeared in Germany in 1981. It is also a registered trade mark since 2003. Many hopeful cancer patients treated by this method have died, at least 140 (see details below). |
| − | + | Germanic New Medicine was invented by barred German physician [[Ryke Geerd Hamer]], who has been prosecuted in several European countries for practicing medicine illegally. Hamer is currently living in Sandefjord, in the south of Norway. His address is the same as his publishing company ''GERMANISCHE NEUE MEDIZIN FORLAG DR. HAMER'' Sandkollveien 11, N-3229 Sandefjord/Norway. In two interviews in September 2007, Hamer stated that he fled from Spain to Norway to escape an arrest warrant from Germany. The warrant was issued on grounds of ''incitement of hatred'' (article 130 of German criminal law), because of Hamer's many public anti-semitic statements in open letters and on web pages, accusing an alleged international Jewish conspiracy (in particular the New York B'nai B'rith) of having killed two billion people by hiding the truth about New Medicine, which Hamer claims can heal 98% of all cancer cases. | |
| + | |||
| + | Since its principles are incompatible with the findings of modern evidence-based medicine, GNM has never been accepted and is widely ignored by the scientific and academic medical community. Hamer spreads his ideas in his books, published by his own publishing company ''Amici di Dirk'', via many different private web pages on the internet and through publications by a number of followers and associations supporting his doctrines. | ||
| + | |||
| + | According to Hamer, every disease of either man, animal or plant was the result of an earlier - not well-defined - ''biological conflict'', obeying to no more than five so-called ''biological laws of nature'' which he claims to have discovered, but which no scientist has been able to confirm as of yet. In addition to this, Hamer states that only the effects of radiation and injuries were not the result of a biological conflict. | ||
| + | |||
| + | GNM is a mainly diagnostic construction and may be seen as a primitive reinvention of some obsolete concepts of psychosomatic medicine, mixed with pseudoscientific, unvalidated tests of Hamer's own invention and a grotesquely erroneous interpretation of CT brain scans. Some of his ideas have already been proposed before (e.g. ''Christian Science'' and anthroposophic medicine etc.). What is usually called disease or symptom, Hamer considers a ''sensible biological program'' (in German: ''sinnvolles biologisches Sonderprogramm''), being the reaction of a healthy organism to alleged biological conflicts. According to Hamer's theory, all severe diseases, such as cancer, can be ''healed'' in 95% of all cases by performing a so-called ''conflictolysis'' according to GNM. Failures of his method or the death of patients are consistently attributed to interventions of ''scholastic medicine'', the use of morphine, or the patient's not being totally committed to GNM. | ||
| + | |||
| + | Hamer does not present any literature supporting his ideas; some of his assertions, however, remind of concepts to be found in anthroposophical medicine and other concepts developed earlier than 1981. No prospective and scientifically controlled clinical test has been made so far to prove a possible efficacy, and no peer-reviewed articles in serious medical journals exist. | ||
| − | |||
| − | |||
| − | |||
==Germanic== | ==Germanic== | ||
| Line 13: | Line 18: | ||
==No published reports about healed cancer patients so far== | ==No published reports about healed cancer patients so far== | ||
| − | No report about healed cancer patients who | + | No report about healed cancer patients who survived a GNM therapy and who were not treated by academic medicine has been published so far, only some anecdotal stories are available. For instance a German person asserts that he survived leukemia eleven times thanks to Hamer's method,<ref>case Joswig, a German extremist right admirer of GNM who claims to be a citizen of ''Deutsches Reich'' (German empire)</ref> another person asserts to have been healed miraculously from an atheroma (this is not cancer), and someone thinks that his torticollis was in fact a non-Hodgkin lymphoma<ref>http://www.pilhar.com/Hamer/NeuMed/Sonderpr/20000101_NonHodgkin.htm</ref>. Admirers and followers of GNM believe that thousands of cancer patients have been healed by GNM. A neutral observer must wonder why they do not show up to support this method. |
==Notable cases of failure== | ==Notable cases of failure== | ||
| − | Many former GNM patients suffering cancer died | + | Many former GNM patients suffering from cancer died. More than 140 persons were known as of 2008. This is documented in different court files and sentences, newspaper articles, reports of relatives, and in the list presented by Aribert Deckers.<ref>http://www.ariplex.com/ama/ama_ham2.htm</ref> Many of them had a good chance to survive as they had a cancer responding well to modern therapies (e.g. testicular cancer, Hodgkin-lymphoma). A detailed presentation of notable cases can be seen here: [[Victims of New Medicine]]. |
| − | Ryke Geerd Hamer developed testicular cancer himself in 1978 (or at the beginning of 1979), but seeked professional help and underwent surgery in a clinic in Tübingen. He survived this miraculously, according to his own opinion he should have had a survival chance of only 2%.<ref>http://www.neue-medizin.de/html/ein_vermachtnis.html</ref> His tumor appeared only two | + | Ryke Geerd Hamer developed testicular cancer himself in 1978 (or at the beginning of 1979), but seeked professional help and underwent surgery in a clinic in Tübingen. He survived this miraculously, according to his own opinion he should have had a survival chance of only 2%.<ref>http://www.neue-medizin.de/html/ein_vermachtnis.html</ref> His tumor appeared only two months after the death of his son Dirk (which was in December 1978), and Hamer was convinced of this event being the cause of his cancer.<ref>http://www.newmedicine.ca/interview.php [...] in 1978 I developed testicular cancer from such a biological conflict, a so-called "loss conflict [...]"</ref>. But cancer needs years to develop, and not two months. His wife died from breast cancer in 1985, a GNM therapy by Hamer was not successful. Hamer said this at the end of 1985 and declared his wife to be his ''first patient after discovering the iron rules of cancer''. |
| − | ==Sceptical view of | + | ==Sceptical view of GNM== |
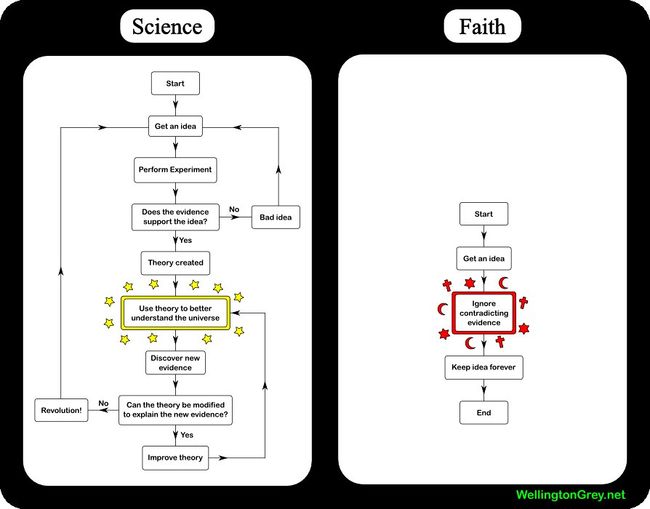
[[image:sciencefaith.jpg|650px|thumb]] | [[image:sciencefaith.jpg|650px|thumb]] | ||
| − | Hamer never published his hypotheses in a scientific paper (his doctoral thesis has nothing to do with it), and apart from an article by Danish holistic physician (now barred) Sören Ventegodt which appeared in a rather unimportant journal<ref>Ventegodt et al. Fulltext: http://www.thescientificworldjournal.com/headeradmin/upload/2005.03.16.pdf</ref> no scientific paper | + | Hamer never published his hypotheses in a scientific paper (his doctoral thesis has nothing to do with it), and apart from an article by Danish holistic physician (now barred) Sören Ventegodt which appeared in a rather unimportant journal<ref>Ventegodt et al. Fulltext: http://www.thescientificworldjournal.com/headeradmin/upload/2005.03.16.pdf</ref>, no scientific paper analysing his method can be found in databases. The author Ventegodt also lost his medical licence in the meantime and has been criticized for working in a pseudoscientific way; furthermore the journal apparently accepts papers after receiving a ''payment''.<ref>http://kasperolsen.wordpress.com/2005/12/19/more-dangerous-pseudo-science/ Ventegodt and pseudoscience</ref> This makes it more difficult to evaluate his ideas. |
| − | + | Hamer does not present scientific proof in favour of his method, and does not present controlled and placebo-controlled prospective studies supporting it. Instead, he shows retrospectively filtered reports and letters of anecdotal value, often written by himself or laypersons. | |
| − | Hamer does never | + | Hamer does never recognise any limit of his medical knowledge (he could not work as physician after 1986) and behaves as an ''expert'' in every branch of medicine, exactly as described by the ''Dunning-Kruger effect''<ref>Justin Kruger, David Dunning (1999), "Unskilled and Unaware of It: How Difficulties in Recognizing One's Own Incompetence Lead to Inflated Self-Assessments". Journal of Personality and Social Psychology 77 (6): 1121–34. PMID 10626367. [http://www.apa.org/journals/features/psp7761121.pdf]</ref><ref>http://en.wikipedia.org/wiki/Dunning-Kruger_effect</ref>, becoming a danger to his patients. |
==External and Internal Contradictions and Obvious Errors== | ==External and Internal Contradictions and Obvious Errors== | ||
| Line 32: | Line 37: | ||
[[image:Mortalitysweden.jpg|thumb|400px|Mortality in Sweden between 1964 and 1996]] | [[image:Mortalitysweden.jpg|thumb|400px|Mortality in Sweden between 1964 and 1996]] | ||
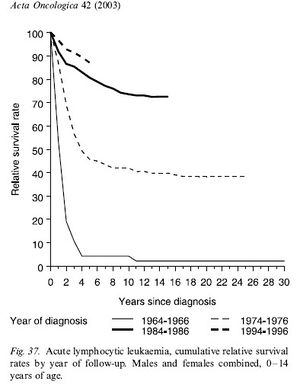
[[image:ALLsweden.jpg|ALL in Sweden Acta Oncol 2003;42|300px|thumb]] | [[image:ALLsweden.jpg|ALL in Sweden Acta Oncol 2003;42|300px|thumb]] | ||
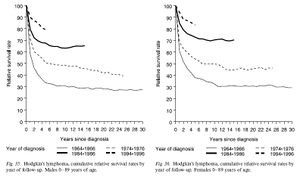
| − | [[image:Hodgkinsweden.jpg| | + | [[image:Hodgkinsweden.jpg|Hodgkin in Sweden Acta Oncol 2003;42|300px|thumb]] |
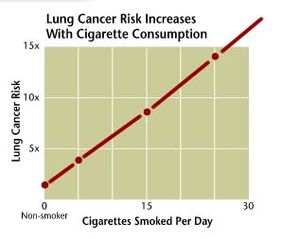
[[image:Smokecancer.jpg|300px|thumb]] | [[image:Smokecancer.jpg|300px|thumb]] | ||
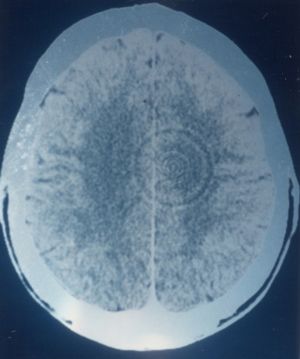
[[image:Yoshihiro.jpg|300px|thumb]] | [[image:Yoshihiro.jpg|300px|thumb]] | ||
| − | Hamer | + | Many of Hamer's different public statements regarding his doctrines are in conflict with each other and in a clear contrast and conflict to the actual knowledge in scientific medicine. |
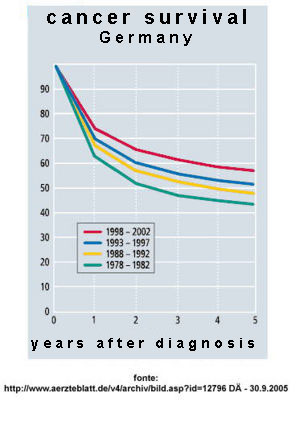
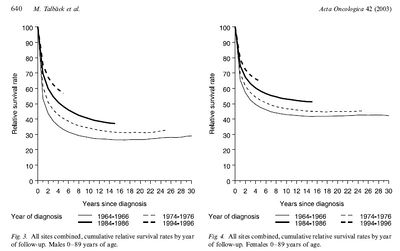
| − | *'''Cancer:''' Hamer states that he was able to cure cancer patients in 98% of all cases but is unable to present a single cured patient. At the same time, it is well known (see his trials, the ''Aribert-Decker-List''<ref>http://www.ariplex.com/ama/ama_ham2.htm</ref> and [[Victims of New Medicine]] / [[Testimonies of former associates of Hamer]]) that many cancer patients following his method died. Some of his statements seem to indicate that the therapeutic principle in new medicine is the so far unknown induction of a ''spontaneous remission'' of cancer after a psychotherapeutical intervention by the patient himself, and assisted by a GNM therapist. The probability of any spontaneous remission is | + | *'''Cancer:''' Hamer states that he was able to cure cancer patients in 98% of all cases but is unable to present a single cured patient. At the same time, it is well known (see his trials, the ''Aribert-Decker-List''<ref>http://www.ariplex.com/ama/ama_ham2.htm</ref> and [[Victims of New Medicine]] / [[Testimonies of former associates of Hamer]]) that many cancer patients following his method died. Some of his statements seem to indicate that the therapeutic principle in new medicine is the so far unknown induction of a ''spontaneous remission'' of cancer after a psychotherapeutical intervention by the patient himself, and assisted by a GNM therapist. The probability of any spontaneous remission, however, is known to be very low, occuring only in about 1:50,000 to 1:140,000 of all cancer cases. These remissions are not only very rare, but at the same time no cure is known today to induce them. Every spontaneous remission is also subject to possible relapses and patients must wait at least five (or more) years until they know that recovery seems to be definitive. At least two different groups of experts are performing research on spontaneous remissions in Germany (one for instance in Nuremberg). At the same time, Hamer declared many times, and still continues to repeat, that ''scientific medicine'' offered only about a 2% survival chance for a cancer patient.<ref>[...] So aber gibt es nur schlechte Verlierer in der dummen und falschen Schulmedizin. Von der strafrechtlichen Seite wollen wir noch gar nicht einmal sprechen., d.h. von der Frage, wer denn für den seit 18 Jahren geübten, vorsätzlichen wissenschaftlichen Massenmord oder Superholokaust an unseren Patienten verantwortlich ist. Denn beim Deutschen Krebsforschungszentrum Heidelberg kann sich doch jeder erkundigen: Bei der "Standesamtsstatistik" (d.h.: Wer lebt wirklich noch nach Chemo-Pseudotherapie ?) findet man, daß nach 5 Jahren 95% der Patienten tot sind, nach 7 Jahren 98%! Das heißt: Man hat alle Patienten regelrecht um ihr Leben betrogen, indem man die Erkenntnisse der neuen Medizin mit ihrer 95%igen (und mehr) Überlebenschance unterdrückt hat! Das war aber nicht ein paar vertrottelte Medizyn-Onkelchens oder saudumme Medienredakteure, xxxxx Richter oder Politiker, sondern das waren die finsteren Mächte der Logenonkelchen und Onkologenbrüderchen, die dieses schlimmste Verbrechen der Menschheitsgeschichte für den Wahn der Weltherrschaft begehen mußten [...] see: http://www.pilhar.com/Hamer/Korrespo/1999/19990415_Hamer_an_Freund_Gallmeier.htm (rif 107)</ref> Hamer sometimes refers to Ulrich Abel, a German expert who never made any statement like this. In reality, modern medicine (evidenced-based medicine and good clinical practice) today offers a survival rate of about 55% (all cases) in Germany<ref>Robert Koch Institut, Germany</ref>, and in other countries, like the USA or Australia, even over 60%<ref>http://annonc.oxfordjournals.org/cgi/reprint/14/suppl_5/v61.pdf (periodo 1990-94, pag. 58)</ref>. National Cancer Institute (USA) indicates a cancer survival of only 20% in 1920. And cancer incidence started to decrease about ten years ago in Germany.<ref>http://www.aerzteblatt.de/v4/archiv/bild.asp?id=12796 (source: http://www.ekr.med.uni-erlangen.de/GEKID/Doc/kid2006.pdf)</ref> |
| − | *Another '''big error:''' Hamer claims that ''1,500 German non-Jewish cancer patients'' were ''killed'' every day by scientific medicine and this can be seen or heard in a video interview dated 2006<ref>http://www.lnc-2010.de/html/neues_deutschland.html</ref> and he continues to assert this claim on different web pages in open letters.<ref>http://www.pilhar.com/Hamer/Korrespo/2007/20070205_Hamer_an_HR3.htm</ref> These data, however, contradict published German cancer statistics of 2002: 420,000 people were newly diagnosed with cancer in that year in Germany, and at the same time 210,000 died because of cancer in 2002. 210000/365=575, Hamer's numbers cannot be correct and 1,500 x 365 = 547,500. This means the number of dead patients would exceed the number of newly | + | *Another '''big error:''' Hamer claims that ''1,500 German non-Jewish cancer patients'' were ''killed'' every day by scientific medicine and this can be seen or heard in a video interview dated 2006<ref>http://www.lnc-2010.de/html/neues_deutschland.html</ref> and he continues to assert this claim on different web pages in open letters.<ref>http://www.pilhar.com/Hamer/Korrespo/2007/20070205_Hamer_an_HR3.htm</ref> These data, however, contradict published German cancer statistics of 2002: 420,000 people were newly diagnosed with cancer in that year in Germany, and at the same time 210,000 died because of cancer in 2002. 210000/365=575, Hamer's numbers cannot be correct and 1,500 x 365 = 547,500. This means the number of dead patients would exceed the number of newly diagnosed patients by 120,000. This is of course impossible. |
| − | *'''Chemotherapy and cancer''': According to | + | *'''Chemotherapy and cancer''': According to Hamer, chemotherapy in cancer treatment would have a fatal effect on every patient and caused the death of many people in the past. However, chemotherapy is mostly used as a coadjuvant therapy combined with surgery or a radiation therapy. Some (not all) cancers are sensitive to particular drugs used. Cancer of this type for instance is Acute Lymphoblastic Leukemia in children, Hodgkin-disease or testicular cancer.<ref>Brandt L, A systematic overview of chemotherapy effects in Hodgkin's disease, Acta oncol 2001;40(2-3):185-97, A systematic review of chemotherapy trials in several tumour types was performed by The Swedish Council of Technology Assessment in Health Care (SBU). The procedures for the evaluation of scientific literature are described separately (Acta Oncol 2001; 40: 155-65). This synthesis of the literature on chemotherapy for Hodgkin's disease (HD) is based on 113 scientific reports including four meta-analyses, 44 randomised studies, 18 prospective studies and 40 retrospective studies. These studies involve 69,196 patients. The conclusions reached can be summarised into the following points: Chemotherapy is of utmost importance for the cure of HD. At early stages, extended field radiotherapy cures most patients. For the majority of patients with relapses after radiotherapy, chemotherapy is curative and the total proportion of cured early stage patients is 75-90%. Chemotherapy in addition to extended field radiotherapy reduces recurrences but does not improve long-term survival. In early stage HD with a large mediastinal mass and/or systemic symptoms, combined treatment with chemotherapy and radiotherapy is recommended. It is likely that chemotherapy will in future play a greater role in the treatment of early stage patients, too, in order to reduce later consequences from extended field radiotherapy. However, this conclusion remains to be better documented in literature. At advanced stages, chemotherapy or a combination of chemotherapy and limited field radiotherapy are effective treatment options and, using the regimens available 10-20 years ago, 40-50% of the patients are cured. Based upon more favourable short-term (three to eight years) results of more recently developed regimens, it can be expected that today a higher proportion of the patients will become long-term survivors. Several chemotherapy regimens containing four to eight drugs are effective in HD. The best regimen considering both antitumour activity and acute and later side-effects is not known. The choice of regimen is probably best done after considering various pre-treatment factors such as the number of poor prognostic signs, concomitant diseases, and individual preferences. The results of chemotherapy are more favourable in young than in elderly patients. The development of less toxic but still effective treatment programmes is therefore particularly important for the elderly. High dose chemotherapy with stem cell support is presently often used in patients who are chemotherapy induction failures, who relapse after a short initial remission or after a longer initial remission and treated initially with seven or eight drugs, or who have had multiple relapses. However, this use is based on data from uncontrolled or small controlled studies, not being fully convincing with respect to effect on survival. Persistent side-effects of treatment are common among long-term survivors, although most patients apparently have a normal life. The relative contributions of chemotherapy and radiotherapy to the persistent effects are not well documented.</ref>. Overall (additional = contribution for chemotherapy for cancer survival is estimated at between 5-10%. |
*'''Tumors in transplanted organs:''' Tumors may also come up in transplanted organs, they were already present in these organs before transplantation (too small to be detected), but it is also known that a tumor can build up after transplantation. After a transplantation, no nerve links this organ to the brain, and therefore the GNM theory of cancer origin fails.<ref>Schwarz A, Renal cell carcinoma in transplant recipients with acquired cystic kidney disease, Clin J Am Soc Nephrol. 2007 Jul;2(4):750-6. Epub 2007 Apr 25 [...] CONCLUSIONS: Renal cell carcinoma occurs often after renal transplantation [...]</ref><ref>Aguilera Tubet C, Multifocal renal cell carcinoma on renal allograft, Actas Urol Esp. 2007 May;31(5):553-5 [...] We report a case of multifocal renal cell carcinoma diagnosed in a kidney grafted 17 years before [...]</ref><ref>Besarani D Urological malignancy after renal transplantation, BJU Int. 2007 Sep;100(3):502-5</ref><ref>Roithmaier S, Incidence of malignancies in heart and/or lung transplant recipients: a single-institution experience, J Heart Lung Transplant. 2007 Aug;26(8):845-9</ref><ref>Ondrus D The incidence of tumours in renal transplant recipients with long-term immunosuppressive therapy, Int Urol Nephrol. 1999;31(4):417-22</ref><ref>Birkeland SA Risk for tumor and other disease transmission by transplantation: a population-based study of unrecognized malignancies and other diseases in organ donors, Transplantation. 2002 Nov 27;74(10):1409-13</ref><ref>Buell JF Donor transmitted malignancies, Ann Transplant. 2004;9(1):53-6</ref> | *'''Tumors in transplanted organs:''' Tumors may also come up in transplanted organs, they were already present in these organs before transplantation (too small to be detected), but it is also known that a tumor can build up after transplantation. After a transplantation, no nerve links this organ to the brain, and therefore the GNM theory of cancer origin fails.<ref>Schwarz A, Renal cell carcinoma in transplant recipients with acquired cystic kidney disease, Clin J Am Soc Nephrol. 2007 Jul;2(4):750-6. Epub 2007 Apr 25 [...] CONCLUSIONS: Renal cell carcinoma occurs often after renal transplantation [...]</ref><ref>Aguilera Tubet C, Multifocal renal cell carcinoma on renal allograft, Actas Urol Esp. 2007 May;31(5):553-5 [...] We report a case of multifocal renal cell carcinoma diagnosed in a kidney grafted 17 years before [...]</ref><ref>Besarani D Urological malignancy after renal transplantation, BJU Int. 2007 Sep;100(3):502-5</ref><ref>Roithmaier S, Incidence of malignancies in heart and/or lung transplant recipients: a single-institution experience, J Heart Lung Transplant. 2007 Aug;26(8):845-9</ref><ref>Ondrus D The incidence of tumours in renal transplant recipients with long-term immunosuppressive therapy, Int Urol Nephrol. 1999;31(4):417-22</ref><ref>Birkeland SA Risk for tumor and other disease transmission by transplantation: a population-based study of unrecognized malignancies and other diseases in organ donors, Transplantation. 2002 Nov 27;74(10):1409-13</ref><ref>Buell JF Donor transmitted malignancies, Ann Transplant. 2004;9(1):53-6</ref> | ||
*'''Inherited cancer:''' In some cancer types it is known for sure that these are inherited and therefore transmitted genetically. One example is familial adenomatous polyposis<ref>http://en.wikipedia.org/wiki/Familial_adenomatous_polyposis</ref> or Xeroderma pigmentosum<ref>http://en.wikipedia.org/wiki/Xeroderma_pigmentosum</ref>. Other cases are Louis-Bar syndrome, Gardner syndrome, Turcot syndrome and familiar form of retinoblastoma. In these cases a ''biological conflict'' as an origin can be excluded. | *'''Inherited cancer:''' In some cancer types it is known for sure that these are inherited and therefore transmitted genetically. One example is familial adenomatous polyposis<ref>http://en.wikipedia.org/wiki/Familial_adenomatous_polyposis</ref> or Xeroderma pigmentosum<ref>http://en.wikipedia.org/wiki/Xeroderma_pigmentosum</ref>. Other cases are Louis-Bar syndrome, Gardner syndrome, Turcot syndrome and familiar form of retinoblastoma. In these cases a ''biological conflict'' as an origin can be excluded. | ||
*'''Cancer caused by virus:''' About 15% of all cancer are caused by viruses (oncovirus), the presence of a viral infection increases incidence. This is the case in high-risk HPV, Burkitt lymphoma and HIV. | *'''Cancer caused by virus:''' About 15% of all cancer are caused by viruses (oncovirus), the presence of a viral infection increases incidence. This is the case in high-risk HPV, Burkitt lymphoma and HIV. | ||
| − | *'''No chemical carcinogens in new medicine:''' The Hamer doctrine allows no chemical carcinogens to exist, they have simply no effect on | + | *'''No chemical carcinogens in new medicine:''' The Hamer doctrine allows no chemical carcinogens to exist, they have simply no effect on tumour formation and smoking does not cause cancer, for instance. Cancer may occur because people were ''in panic'' after hearing that carcinogens like asbestos were harmful. |
| − | *'''No metastasis in GNM:''' According to the same doctrine metastases | + | *'''No metastasis in GNM:''' According to the same doctrine metastases do not exist and allegedly were never proved by scientific medicine. Tumours appearing after a first tumour were due to the panic of the patient who, suffering, was producing new tumours. Also, isolate tumor cells would not be detectable in blood, especially not in arterial blood.<ref>http://www.neue-medizin.de/html/3__naturgesetz.html</ref> Many scientific articles tell us the opposite. Since 1869 (more than 130 years ago), it is known that tumors emit single cancer cells or groups of them into the blood, and every day a tumor may emit millions of cells even if only a minority may survive (perhaps 0,01%) and be the source of a distant metastasis<ref>Wong LS, Detection of circulating tumour cells and nodal metastasis by reverse transcriptase-polymerase chain reaction technique, Br J surg 2005 Vol 84 (6) 834, In the search for occult metastases in lymph nodes or circulating tumour cells, a reverse transcriptase-polymerase chain reaction (RT-PCR) assay was developed to detect tumour-specific splice variants of the transcript of the CD44 gene. The assay was highly sensitive and could detect ten tumour cell per 10(5) leucocytes. METHODS: RNA was purified from peripheral blood (n = 24) and regional lymph nodes (n = 14) from patients with colorectal cancer. Complementary DNA was made and amplified using primers specific for the CD44 gene. Southern blotting with exon-specific probes was used to enhance the sensitivity. RESULTS: Tumour cells were detected in peripheral blood samples in four patients and lymph nodes in nine, in one of whom conventional histology had not detected tumour cells. CONCLUSION: This technique may be useful in the early diagnosis of primary or metastatic tumours, in assessing prognosis and in detecting residual disease after treatment.</ref><ref>Sadahiro S, Detection of Carcinoembryonic Antigen Messenger RNA-Expressing Cells in Peripheral Blood 7 Days After Curative Surgery is a Novel Prognostic Factor in Colorectal Cancer, Ann Surg Oncol 2007 jan 3, BACKGROUND: The significance of detection of circulating cancer cells in blood during surgery in patients with colorectal cancer (CRC) remains controversial. Experimental study revealed that the cancer cells injected from the vein disappeared completely until 7 days. The aim of this study was to clarify that the detection of circulating cancer cells in blood taken later than 7 days after curative surgery may be a prognostic factor. METHODS: Two hundred consecutive patients with CRC who underwent potentially curative surgery were the subjects. Peripheral blood was collected between 7 and 10 days after resection. Cancer cells were detected using reverse transcriptase-polymerase chain reaction targeting carcinoembryonic antigen (CEA) messenger RNA (mRNA). The median follow-up period was 52 months (range: 34-69 months). RESULTS: The overall positive incidence of CEA mRNA was 22%. Detection of CEA mRNA was not significantly related to conventional clinicopathological findings. Recurrence has been confirmed in 55 patients (28%). The recurrence rate was significantly higher in patients with rectal cancer, deep penetration, lymph node metastasis, preoperative chemoradiotherapy and positive CEA mRNA. The CEA mRNA positive patients showed significantly poorer disease free survival (DFS) and overall survival (OS) than the negative patients (DFS, P=0.007; OS, P=0.04). Multivariate analysis revealed that the positive expression of CEA mRNA (P < 0.01) as well as the tumor location and TNM stage classification was identified as the significant risk factors for recurrence. CONCLUSIONS: Detection of CEA mRNA expressing cells in peripheral blood 7 days after curative surgery is a novel independent factor predicting recurrence in patients with CRC.</ref><ref>Castells A, Detection of colonic cells in peripheral blood of colorectal cancer patients by means of reverse transcriptase and polymerase chain reaction, Br J Cancer, 1998 78(10) 1368, Circulating tumour cells play a central role in the metastatic process, but little is known about the relationship between this cellular subpopulation and the development of secondary disease. This study was aimed at assessing the presence of colonic cells in peripheral blood of patients with colorectal cancer in different evolutionary stages, by means of reverse transcriptase polymerase chain reaction (RT-PCR) targeted to carcinoembryonic antigen (CEA) mRNA. In vitro sensitivity was established in a recovery experiment by preparing serial colorectal cancer cell dilutions. Thereafter, 95 colorectal cancer patients and a control group including healthy subjects (n = 11), patients with other gastrointestinal neoplasms (n = 11) or inflammatory bowel disease (n = 9) were analysed. Specific cDNA primers for CEA transcripts were used to apply RT-PCR to peripheral blood samples. Tumour cells were detected down to five cells per 10 ml blood, thus indicating a sensitivity limit of approximately one tumour cell per 10(7) white blood cells. CEA mRNA expression was detected in 39 out of 95 colorectal cancer patients (41.1%), there being a significant correlation with the presence of distant metastases at inclusion. None of the healthy volunteers and only 1 of 11 patients (9.1%) with other gastrointestinal neoplasms had detectable CEA mRNA in peripheral blood. By contrast, CEA mRNA was detected in five of the nine patients (55.6%) with inflammatory bowel disease. These results confirm that it is feasible to amplify CEA mRNA in the peripheral blood, its presence being almost certainly derived from circulating malignant cells in colorectal cancer patients. However, CEA mRNA detectable in blood of patients with inflammatory bowel disease suggests the presence of circulating non-neoplastic colonic epithelial cells.</ref><ref>Nakamori S, Genetic detection of colorectal cancer cells in circulation and lymph nodes, Dis Colon Rectum 1997 40(10 sup) S29-36, PURPOSE: This study was undertaken to investigate the clinical implications of detection of genetic alterations in blood and lymph nodes in colorectal cancer patients. METHODS: The reverse transcriptase polymerase chain reaction product of the cytokeratin gene in blood was examined as a cancer cell-specific expression in 35 colorectal cancer patients. The K-ras or p53 gene mutations in the lymph nodes histopathologically negative for metastasis were studied by the mutant-allele-specific amplification method in 26 colorectal cancer patients. RESULTS: The reverse transcriptase polymerase chain reaction assay was able to detect a cytokeratin reverse transcriptase polymerase chain reaction product at a concentration from a single to ten colon cancer cells per 10(6) normal peripheral blood mononuclear cells. Cytokeratin reverse transcriptase polymerase chain reaction products were detected in nine patients' blood samples, although none of the samples were cytologically detectable. The blood's cytokeratin positivity correlated with the invasive mode of the tumor (P < 0.05) and the presence of distant metastasis (P < 0.01). Two (50 percent) of four patients whose blood was positive for cytokeratin had recurrences. Of 17 patients with the K-ras or p53 gene mutation in primary tumors, 9 (53 percent) had the corresponding mutations in lymph nodes. Mutation positivity in lymph nodes correlated with the presence of lymphatic invasion of the primary tumor (P < 0.05). All patients with mutation-negative lymph nodes remained disease-free for more than two years after surgery. CONCLUSION: Detection of cytokeratin reverse transcriptase polymerase chain reaction products in the blood and K-ras or p53 gene mutations in the lymph nodes histologically negative for metastasis may be applicable for clinical use, despite some limitations, and may serve as a useful clinical factor for stratifying patients who are at high or low risk for recurrence after surgery.</ref><ref>Iinuma H, Detection of tumor cells in blood using CD45 magnetic cell separation followed by nested mutant allele-specific amplification of p53 and K-ras genes in patients with colorectal cancer, Int J Cancer 2000 89(4) 337, |
A new method for detecting circulating tumor cells that is based on magnetic-activated cell separation (MACS) and nested mutant allele-specific amplification (nested MASA) was evaluated in patients with colorectal cancer using the p53 and K-ras genes as genetic markers. By negative selection with anti-CD45 monoclonal antibody-conjugated supermagnetic microbeads, the proportion of tumor cells was enriched 9-fold. By the combination of MACS and nested MASA, 10 tumor cells in 10(7) normal peripheral blood mononuclear cells could be detected without false-positives. Using this method, we examined blood taken from the tumor drainage veins of 23 patients with colorectal cancer. Eighty-seven percent (20/23) of primary tumor tissues showed p53 and/or K-ras gene mutations. Forty-five percent (9/20) of patients with p53 and/or K-ras mutations in the primary tumor showed the same mutated genes in the blood samples. There was a significant association between the presence of p53 and K-ras gene mutation in the blood and tumor size, depth of invasion, and venous invasion. Blood gene mutation was detected in 80% (4/5) of samples from patients with synchronous liver metastases. Sixty percent (3/5) of patients with mutant genes in the blood developed asynchronous liver metastases after surgery. The overall survival of patients with p53 and/or K-ras gene mutation-positive findings in blood was significantly shorter than that of patients testing negative on Kaplan-Meier analysis. Our results suggest that the method may be useful for reliable detection of tumor cells circulating in the blood and may help to identify patients at high risk for relapse. Copyright 2000 Wiley-Liss, Inc.</ref><ref>Wang JY, Molecular detection of APC, K- ras, and p53 mutations in the serum of colorectal cancer patients as circulating biomarkers, World J Surg 2004 28(7) 721, Early detection of tumor DNA in serum/plasma prior to the development of recurrence or metastases could help improve the outcome of patients with colorectal cancer (CRC) after tumor resection. Recent advances in the detection of tumor DNA in the serum/plasma has opened up numerous new areas for investigation and new possibilities for molecular diagnosis. APC and K- ras mutations are considered to be early-stage developments of CRCs, whereas p53 mutations are thought to be relatively late events in the tumorigenesis of CRCs. The aim of this study was to search for the presence of genetic mutations in the DNA extracted from the serum of CRC patients and healthy subjects. We simultaneously evaluate the significance of APC, K- ras, and p53 gene mutations in cancer tissues and their paired serum samples of 104 CRC patients by polymerase chain reaction-single strand conformation polymorphism analysis (PCR-SSCP) followed by direct sequencing. Additionally, analysis was carried out to detect the serum carcinoembryonic antigen (CEA) levels in CRC patients. Overall, we found at least one of the gene mutations in tumor tissues from 75% (78/104) of the CRC patients. Comparison of the three molecular markers showed that the detection rates in the serum were 30.4%, 34.0%, and 34.2% for APC, K- ras, and p53 genes, respectively. Of these patients, 46.2% (36/78) were identified as having positive serum results, whereas all healthy controls remained negative. The overall positive tumor DNA detection rates in the serum were 0% (0/7) for Dukes' A classification, 22.4% (11/49) for Dukes' B, 48.7% (19/39) for Dukes' C, and 66.7% (6/9) for Dukes' D. The detection rate increased as the tumor stage progressed ( p = 0.012). Concurrently, a significant difference was observed between lymph node metastases and positive serum tumor DNA detection ( p < 0.001). A significantly higher postoperative metastasis/recurrence rate in patients harboring gene mutations with serum tumor DNA than those without serum tumor DNA was also demonstrated ( p < 0.001). However, no significant correlation between the postoperative metastasis/recurrence and serum CEA levels was observed ( p = 0.247). These data suggest that the identification of circulating tumor DNA using the molecular detection of APC, K- ras, and p53 gene mutations is a potential tool for early detection of postoperative recurrence/metastases. Moreover, these genes may be potential molecular markers of poor clinical outcome in CRC patients.</ref><ref>Wang JY, Molecular detection of circulating tumor cells in the peripheral blood of patients with colorectal cancer using RT-PCR: significance of the prediction of postoperative metastasis, World J Surg 2006 june 30(6) 1007, | A new method for detecting circulating tumor cells that is based on magnetic-activated cell separation (MACS) and nested mutant allele-specific amplification (nested MASA) was evaluated in patients with colorectal cancer using the p53 and K-ras genes as genetic markers. By negative selection with anti-CD45 monoclonal antibody-conjugated supermagnetic microbeads, the proportion of tumor cells was enriched 9-fold. By the combination of MACS and nested MASA, 10 tumor cells in 10(7) normal peripheral blood mononuclear cells could be detected without false-positives. Using this method, we examined blood taken from the tumor drainage veins of 23 patients with colorectal cancer. Eighty-seven percent (20/23) of primary tumor tissues showed p53 and/or K-ras gene mutations. Forty-five percent (9/20) of patients with p53 and/or K-ras mutations in the primary tumor showed the same mutated genes in the blood samples. There was a significant association between the presence of p53 and K-ras gene mutation in the blood and tumor size, depth of invasion, and venous invasion. Blood gene mutation was detected in 80% (4/5) of samples from patients with synchronous liver metastases. Sixty percent (3/5) of patients with mutant genes in the blood developed asynchronous liver metastases after surgery. The overall survival of patients with p53 and/or K-ras gene mutation-positive findings in blood was significantly shorter than that of patients testing negative on Kaplan-Meier analysis. Our results suggest that the method may be useful for reliable detection of tumor cells circulating in the blood and may help to identify patients at high risk for relapse. Copyright 2000 Wiley-Liss, Inc.</ref><ref>Wang JY, Molecular detection of APC, K- ras, and p53 mutations in the serum of colorectal cancer patients as circulating biomarkers, World J Surg 2004 28(7) 721, Early detection of tumor DNA in serum/plasma prior to the development of recurrence or metastases could help improve the outcome of patients with colorectal cancer (CRC) after tumor resection. Recent advances in the detection of tumor DNA in the serum/plasma has opened up numerous new areas for investigation and new possibilities for molecular diagnosis. APC and K- ras mutations are considered to be early-stage developments of CRCs, whereas p53 mutations are thought to be relatively late events in the tumorigenesis of CRCs. The aim of this study was to search for the presence of genetic mutations in the DNA extracted from the serum of CRC patients and healthy subjects. We simultaneously evaluate the significance of APC, K- ras, and p53 gene mutations in cancer tissues and their paired serum samples of 104 CRC patients by polymerase chain reaction-single strand conformation polymorphism analysis (PCR-SSCP) followed by direct sequencing. Additionally, analysis was carried out to detect the serum carcinoembryonic antigen (CEA) levels in CRC patients. Overall, we found at least one of the gene mutations in tumor tissues from 75% (78/104) of the CRC patients. Comparison of the three molecular markers showed that the detection rates in the serum were 30.4%, 34.0%, and 34.2% for APC, K- ras, and p53 genes, respectively. Of these patients, 46.2% (36/78) were identified as having positive serum results, whereas all healthy controls remained negative. The overall positive tumor DNA detection rates in the serum were 0% (0/7) for Dukes' A classification, 22.4% (11/49) for Dukes' B, 48.7% (19/39) for Dukes' C, and 66.7% (6/9) for Dukes' D. The detection rate increased as the tumor stage progressed ( p = 0.012). Concurrently, a significant difference was observed between lymph node metastases and positive serum tumor DNA detection ( p < 0.001). A significantly higher postoperative metastasis/recurrence rate in patients harboring gene mutations with serum tumor DNA than those without serum tumor DNA was also demonstrated ( p < 0.001). However, no significant correlation between the postoperative metastasis/recurrence and serum CEA levels was observed ( p = 0.247). These data suggest that the identification of circulating tumor DNA using the molecular detection of APC, K- ras, and p53 gene mutations is a potential tool for early detection of postoperative recurrence/metastases. Moreover, these genes may be potential molecular markers of poor clinical outcome in CRC patients.</ref><ref>Wang JY, Molecular detection of circulating tumor cells in the peripheral blood of patients with colorectal cancer using RT-PCR: significance of the prediction of postoperative metastasis, World J Surg 2006 june 30(6) 1007, | ||
BACKGROUND: Approximately 20%-45% of colorectal cancer (CRC) patients ultimately develop local recurrence or metastasis following curative surgical resection. The latter is caused by tumor cells shed from the primary carcinoma prior to or during operation, currently undetected by standard clinical staging. Fortunately, the presence of tumor cells in peripheral blood can be detected by molecular methods and is being regarded increasingly as a clinically relevant prognostic factor. MATERIALS AND METHODS: To detect the presence of circulating tumor cells and evaluate their relationship to postoperative metastatic relapse, we simultaneously examined human telomerase reverse transcriptase (hTERT), cytokeratin-19 (CK-19), cytokeratin-20 (CK-20), and carcinoembryonic antigen (CEA) mRNA (messenger RNA) in the peripheral blood of 72 CRC patients and 30 healthy individuals. Using a reverse-transcriptase polymerase chain reaction (RT-PCR), these tumor-related mRNAs were amplified; in addition, analyses were carried out for their correlation with patients' clinicopathologic features, as well as the occurrence of postoperative metastasis. RESULTS: In RT-PCR analysis of the peripheral blood, 69.4% (50 out of 72), 66.7% (48 out of 72), 52.8% (38 out of 72), and 72.2% (52 out of 72) of CRC patients were positive for hTERT, CK-19, CK-20, and CEA mRNA respectively. All 30 healthy individuals were negative for hTERT and CEA mRNA expression, while 2 were positive for either CK-19 mRNA or CK-20 mRNA expression. The detection of CEA mRNA was significantly correlated with depth of tumor invasion (P=0.012), vessel invasion (P=0.035), TNM stage (P<0.0001), and postoperative metastasis (P<0.0001), while positive hTERT mRNA was correlated with TNM stage (P=0.037) and CK-19 was correlated with depth of tumor invasion (P=0.039) and postoperative metastasis (P=0.017). In addition, multivariate logistic regression showed that only CEA mRNA was an independent and significant predictor of postoperative metastasis (P=0.006). Our findings suggest that CEA mRNA may be a more reliable marker than hTERT, CK-19, and CK-20 for the detection of circulating cancer cells in the peripheral blood of CRC patients. CONCLUSIONS: Using RT-PCR for the detection of CEA mRNA is feasible and may be a promising tool for early detection of micrometastatic circulating tumor cells in CRC patients. CRC patients expressing positive CEA mRNA in peripheral blood have a significantly higher risk of postoperative metastasis. Nevertheless, confirmation of CEA mRNA as a prognostic predictive factor requires the continuation of patient follow-up.</ref><ref>Guadagni F, Detection of blood-borne cells in colorectal cancer patients by nested reverse transcription-polymerase chain reaction for carcinoembryonic antigen messenger RNA: longitudinal analyses and demonstration of its potential importance as an adjunct to multiple serum markers, Cancer res 2001 15 61(6) 2523, The use of reverse transcription-PCR (RT-PCR) to analyze cells in the blood of cancer patients for the detection of mRNA expressed in tumor cells has implications for both the prognosis and the monitoring of cancer patients for the efficacy of established or experimental therapies. Carcinoembryonic antigen (CEA) is expressed on approximately 95% of colorectal, gastric, and pancreatic tumors, and on the majority of breast, non-small cell lung, and head and neck carcinomas. CEA shed in serum is useful as a marker in only approximately 50% of colorectal cancer patients and rarely is shed by some other carcinoma types. RT-PCR has been used previously to detect CEA mRNA in cells in the blood and lymph nodes of cancer patients. Under the assay conditions validated in the studies reported here, 34 of 51 (67%) patients with different stages of colorectal cancer had blood cells that were positive by RT-PCR for CEA mRNA, whereas none of 18 patients with colonic polyps were positive; 2 of 60 apparently healthy individuals (who were age and sex matched with the carcinoma patients and were part of a colon cancer screening program as controls) were marginally positive. The results of CEA PCR in the blood of the carcinoma patients and the other groups showed strong statistical correlation with the disease (P2 < 0.0001). Analyses were carried out to detect both serum CEA protein levels and CEA mRNA in blood cells of colorectal carcinoma patients by RT-PCR. For all stages of disease, 18 of 51 patients (35%) were positive for serum CEA, whereas 35 of 51 (69%) were positive by RT-PCR. More importantly, only 5 of 23 (20%) of stage B and C colorectal cancer patients were positive for serum CEA, whereas 16 of 23 (70%) were positive by RT-PCR. The use of two other serum markers (CA19.9 and CA72-4) for colorectal cancer in combination with serum CEA scored two additional patients as positive; both were positive by RT-PCR for CEA mRNA. Pilot long-term longitudinal studies conducted before and after surgery identified some patients with CEA mRNA in blood cells that were negative for all serum markers, who eventually developed clinical metastatic disease. The studies reported here are the first to correlate RT-PCR results for CEA mRNA in blood cells with one or more serum markers for patients with different stages of colorectal cancer, and are the first long-term longitudinal studies to use RT-PCR to detect CEA mRNA in blood cells of cancer patients. Larger cohorts will be required in future studies to define the impact, if any, of this technology on prognosis and/or disease monitoring.</ref><ref>Guller U, Disseminated single tumor cells as detected by real-time quantitative polymerase chain reaction represent a prognostic factor in patients undergoing surgery for colorectal cancer, Ann Surg 2002 dec 236(6) 768, OBJECTIVE: To evaluate the clinical relevance of real-time quantitative polymerase chain reaction (qPCR) detection of CEA and CK20 transcripts, as potentially related to tumor cell dissemination, in blood and peritoneal lavage from patients undergoing surgery for colorectal cancer. SUMMARY BACKGROUND DATA: Dissemination of single colorectal cancer cells in the peritoneal cavity, as well as in tumor drainage and peripheral blood vessels, might play a role in the metastasis process, thus affecting the clinical course. However, this phenomenon needs further elucidation. METHODS: In a prospective study the authors evaluated the potential of qPCR in the detection of CEA and/or CK20 transcripts in the peritoneal lavage fluid and in the peripheral and mesenteric venous blood of 39 patients undergoing curative resection for colorectal cancer. Peritoneal lavage and peripheral blood was sampled before and after tumor resection; mesenteric venous blood was sampled from the major tumor-draining vein immediately before clamping. After RNA extraction and reverse transcription, qPCR was performed using specific cDNA primers and probes for CEA and CK20. The dichotomous results from the qPCR were used as a predictor along with other covariates in Cox proportional hazard regression models of long-term outcome (disease-free survival and overall survival). RESULTS: Of 39 patients, 11 were positive. The median follow-up at analysis was 31 months for all patients. The dichotomous qPCR covariate was significant, with P =.001 and.0035 for disease-free survival and overall survival, respectively, in the proportional hazard regression models with only qPCR. In seven patients, disseminated colorectal cancer cells were found in the peritoneal lavage fluid but not in blood specimens; five of these patients (71%) had recurrence. CONCLUSIONS: These data suggest that detection of mRNA coding for CEA and/or CK20 using qPCR has potential clinical utility as a prognostic marker and should be evaluated in larger clinical studies. Identification of patients at high risk for metastatic disease after curative resection of colorectal cancer might be improved by analyzing peritoneal lavage specimens in addition to blood samples. This is based on the observation that in more than half of qPCR-positive patients, disseminated colorectal cancer cells were detected in peritoneal lavage specimens but not in blood samples, and that 71% of them had recurrence.</ref><ref>Elshimali YI, The clinical significance of circulating tumor cells in the peripheral blood, Diagn Mol Pathol 2006 15(4) 187, Tumors launch malignant cells into the circulation continuously. In early stages, the immune surveillance system eliminates these cells from the circulation, but at later times they may persist longer and be detected. The first recorded evidence of the presence of circulating tumor cells in the peripheral blood of cancer patients was documented in 1869. Now, modern molecular biologic and cell sorting techniques make their detection and characterization more practicable. This review will consider the methods currently available for their detection and characterization, and the clinical implications of their presence in various malignant conditions.</ref><ref>Mejean A, Detection of circulating prostate derived cells in patients with prostate adenocarcinoma is an independent risk factor for tumor recurrence, J Urol 2000 june 163 (6) 2022, PURPOSE: To determine whether the presence of prostate-derived cells in the peripheral blood circulation is a marker of prostate cancer and to define the clinical impact of the test. MATERIALS AND METHODS: We tested the peripheral blood of 99 patients with prostate adenocarcinoma (PAC), 79 of them undergoing radical prostatectomy, and 92 controls (31 healthy volunteers, 50 patients with adenoma and 11 with prostatitis) using a highly controlled procedure including reverse-transcriptase polymerase chain reaction (RT-PCR) targeted to prostate-specific antigen (PSA) mRNA. Patients were followed for 26 +/- 12 (range: 4 to 49) months. Forty tumor tissues were analyzed by immunohistochemistry for expression of p53 and E-cadherin antigens. RESULTS: Thirty three (33%) patients with PAC and 2 (2%) controls scored positive (p <0.0001) for the test. Detection of circulating prostatic cells was associated with development of metastases (p <0. 001), with relapse (p <0.001) and with a serum PSA level at diagnosis higher than 15 ng./ml. (p = 0.009). The rate of development of metastases according to time was significantly higher in patients who scored positive for the test (p <0.04). In a multivariate analysis, only the RT-PCR test was an independent risk factor associated with relapse (RR: 6.7). Finally, E-cadherin expression was significantly lower in the tumor tissues of positive patients as compared with those who scored negative for the test (p <0.01). CONCLUSIONS: This RT-PCR procedure, performed at diagnosis and with appropriate controls, is a clinically useful assay in evaluating the risk of tumor recurrence after radical prostatectomy in patients with PAC.</ref><ref>Massimo Cristofanilli,Circulating Tumor Cells, Disease Progression, and Survival in Metastatic Breast Cancer, NEJM Vol 351 august 2004, http://content.nejm.org/cgi/content/abstract/351/8/78</ref>. Often the PCT-technique is used known from the genetic fingerprints. A newer work (december 2007) by Mehmet Toner about an automat registering single cancer cells: <ref>*http://www.istitutoncologicoveneto.it/it/rassegna/2012/201207-02.pdf (nature medicine No 20 december 2007</ref>. Hamer instead believes that there were no studies showing these cancer cells in arterial blood, but this is false and irrelevant because the presence of isolated cancer cells in venous blood of the controlateral side of the tumors can't be explained either. Some articles (out of many) showing cancer cells in arterial blood are: <ref>Yoshihiro Hayata M.D, Significance of Carcinoma Cells in the Blood Relative to Surgery of Pulmonary Carcinoma, Chest 1964;46:51-60.) | BACKGROUND: Approximately 20%-45% of colorectal cancer (CRC) patients ultimately develop local recurrence or metastasis following curative surgical resection. The latter is caused by tumor cells shed from the primary carcinoma prior to or during operation, currently undetected by standard clinical staging. Fortunately, the presence of tumor cells in peripheral blood can be detected by molecular methods and is being regarded increasingly as a clinically relevant prognostic factor. MATERIALS AND METHODS: To detect the presence of circulating tumor cells and evaluate their relationship to postoperative metastatic relapse, we simultaneously examined human telomerase reverse transcriptase (hTERT), cytokeratin-19 (CK-19), cytokeratin-20 (CK-20), and carcinoembryonic antigen (CEA) mRNA (messenger RNA) in the peripheral blood of 72 CRC patients and 30 healthy individuals. Using a reverse-transcriptase polymerase chain reaction (RT-PCR), these tumor-related mRNAs were amplified; in addition, analyses were carried out for their correlation with patients' clinicopathologic features, as well as the occurrence of postoperative metastasis. RESULTS: In RT-PCR analysis of the peripheral blood, 69.4% (50 out of 72), 66.7% (48 out of 72), 52.8% (38 out of 72), and 72.2% (52 out of 72) of CRC patients were positive for hTERT, CK-19, CK-20, and CEA mRNA respectively. All 30 healthy individuals were negative for hTERT and CEA mRNA expression, while 2 were positive for either CK-19 mRNA or CK-20 mRNA expression. The detection of CEA mRNA was significantly correlated with depth of tumor invasion (P=0.012), vessel invasion (P=0.035), TNM stage (P<0.0001), and postoperative metastasis (P<0.0001), while positive hTERT mRNA was correlated with TNM stage (P=0.037) and CK-19 was correlated with depth of tumor invasion (P=0.039) and postoperative metastasis (P=0.017). In addition, multivariate logistic regression showed that only CEA mRNA was an independent and significant predictor of postoperative metastasis (P=0.006). Our findings suggest that CEA mRNA may be a more reliable marker than hTERT, CK-19, and CK-20 for the detection of circulating cancer cells in the peripheral blood of CRC patients. CONCLUSIONS: Using RT-PCR for the detection of CEA mRNA is feasible and may be a promising tool for early detection of micrometastatic circulating tumor cells in CRC patients. CRC patients expressing positive CEA mRNA in peripheral blood have a significantly higher risk of postoperative metastasis. Nevertheless, confirmation of CEA mRNA as a prognostic predictive factor requires the continuation of patient follow-up.</ref><ref>Guadagni F, Detection of blood-borne cells in colorectal cancer patients by nested reverse transcription-polymerase chain reaction for carcinoembryonic antigen messenger RNA: longitudinal analyses and demonstration of its potential importance as an adjunct to multiple serum markers, Cancer res 2001 15 61(6) 2523, The use of reverse transcription-PCR (RT-PCR) to analyze cells in the blood of cancer patients for the detection of mRNA expressed in tumor cells has implications for both the prognosis and the monitoring of cancer patients for the efficacy of established or experimental therapies. Carcinoembryonic antigen (CEA) is expressed on approximately 95% of colorectal, gastric, and pancreatic tumors, and on the majority of breast, non-small cell lung, and head and neck carcinomas. CEA shed in serum is useful as a marker in only approximately 50% of colorectal cancer patients and rarely is shed by some other carcinoma types. RT-PCR has been used previously to detect CEA mRNA in cells in the blood and lymph nodes of cancer patients. Under the assay conditions validated in the studies reported here, 34 of 51 (67%) patients with different stages of colorectal cancer had blood cells that were positive by RT-PCR for CEA mRNA, whereas none of 18 patients with colonic polyps were positive; 2 of 60 apparently healthy individuals (who were age and sex matched with the carcinoma patients and were part of a colon cancer screening program as controls) were marginally positive. The results of CEA PCR in the blood of the carcinoma patients and the other groups showed strong statistical correlation with the disease (P2 < 0.0001). Analyses were carried out to detect both serum CEA protein levels and CEA mRNA in blood cells of colorectal carcinoma patients by RT-PCR. For all stages of disease, 18 of 51 patients (35%) were positive for serum CEA, whereas 35 of 51 (69%) were positive by RT-PCR. More importantly, only 5 of 23 (20%) of stage B and C colorectal cancer patients were positive for serum CEA, whereas 16 of 23 (70%) were positive by RT-PCR. The use of two other serum markers (CA19.9 and CA72-4) for colorectal cancer in combination with serum CEA scored two additional patients as positive; both were positive by RT-PCR for CEA mRNA. Pilot long-term longitudinal studies conducted before and after surgery identified some patients with CEA mRNA in blood cells that were negative for all serum markers, who eventually developed clinical metastatic disease. The studies reported here are the first to correlate RT-PCR results for CEA mRNA in blood cells with one or more serum markers for patients with different stages of colorectal cancer, and are the first long-term longitudinal studies to use RT-PCR to detect CEA mRNA in blood cells of cancer patients. Larger cohorts will be required in future studies to define the impact, if any, of this technology on prognosis and/or disease monitoring.</ref><ref>Guller U, Disseminated single tumor cells as detected by real-time quantitative polymerase chain reaction represent a prognostic factor in patients undergoing surgery for colorectal cancer, Ann Surg 2002 dec 236(6) 768, OBJECTIVE: To evaluate the clinical relevance of real-time quantitative polymerase chain reaction (qPCR) detection of CEA and CK20 transcripts, as potentially related to tumor cell dissemination, in blood and peritoneal lavage from patients undergoing surgery for colorectal cancer. SUMMARY BACKGROUND DATA: Dissemination of single colorectal cancer cells in the peritoneal cavity, as well as in tumor drainage and peripheral blood vessels, might play a role in the metastasis process, thus affecting the clinical course. However, this phenomenon needs further elucidation. METHODS: In a prospective study the authors evaluated the potential of qPCR in the detection of CEA and/or CK20 transcripts in the peritoneal lavage fluid and in the peripheral and mesenteric venous blood of 39 patients undergoing curative resection for colorectal cancer. Peritoneal lavage and peripheral blood was sampled before and after tumor resection; mesenteric venous blood was sampled from the major tumor-draining vein immediately before clamping. After RNA extraction and reverse transcription, qPCR was performed using specific cDNA primers and probes for CEA and CK20. The dichotomous results from the qPCR were used as a predictor along with other covariates in Cox proportional hazard regression models of long-term outcome (disease-free survival and overall survival). RESULTS: Of 39 patients, 11 were positive. The median follow-up at analysis was 31 months for all patients. The dichotomous qPCR covariate was significant, with P =.001 and.0035 for disease-free survival and overall survival, respectively, in the proportional hazard regression models with only qPCR. In seven patients, disseminated colorectal cancer cells were found in the peritoneal lavage fluid but not in blood specimens; five of these patients (71%) had recurrence. CONCLUSIONS: These data suggest that detection of mRNA coding for CEA and/or CK20 using qPCR has potential clinical utility as a prognostic marker and should be evaluated in larger clinical studies. Identification of patients at high risk for metastatic disease after curative resection of colorectal cancer might be improved by analyzing peritoneal lavage specimens in addition to blood samples. This is based on the observation that in more than half of qPCR-positive patients, disseminated colorectal cancer cells were detected in peritoneal lavage specimens but not in blood samples, and that 71% of them had recurrence.</ref><ref>Elshimali YI, The clinical significance of circulating tumor cells in the peripheral blood, Diagn Mol Pathol 2006 15(4) 187, Tumors launch malignant cells into the circulation continuously. In early stages, the immune surveillance system eliminates these cells from the circulation, but at later times they may persist longer and be detected. The first recorded evidence of the presence of circulating tumor cells in the peripheral blood of cancer patients was documented in 1869. Now, modern molecular biologic and cell sorting techniques make their detection and characterization more practicable. This review will consider the methods currently available for their detection and characterization, and the clinical implications of their presence in various malignant conditions.</ref><ref>Mejean A, Detection of circulating prostate derived cells in patients with prostate adenocarcinoma is an independent risk factor for tumor recurrence, J Urol 2000 june 163 (6) 2022, PURPOSE: To determine whether the presence of prostate-derived cells in the peripheral blood circulation is a marker of prostate cancer and to define the clinical impact of the test. MATERIALS AND METHODS: We tested the peripheral blood of 99 patients with prostate adenocarcinoma (PAC), 79 of them undergoing radical prostatectomy, and 92 controls (31 healthy volunteers, 50 patients with adenoma and 11 with prostatitis) using a highly controlled procedure including reverse-transcriptase polymerase chain reaction (RT-PCR) targeted to prostate-specific antigen (PSA) mRNA. Patients were followed for 26 +/- 12 (range: 4 to 49) months. Forty tumor tissues were analyzed by immunohistochemistry for expression of p53 and E-cadherin antigens. RESULTS: Thirty three (33%) patients with PAC and 2 (2%) controls scored positive (p <0.0001) for the test. Detection of circulating prostatic cells was associated with development of metastases (p <0. 001), with relapse (p <0.001) and with a serum PSA level at diagnosis higher than 15 ng./ml. (p = 0.009). The rate of development of metastases according to time was significantly higher in patients who scored positive for the test (p <0.04). In a multivariate analysis, only the RT-PCR test was an independent risk factor associated with relapse (RR: 6.7). Finally, E-cadherin expression was significantly lower in the tumor tissues of positive patients as compared with those who scored negative for the test (p <0.01). CONCLUSIONS: This RT-PCR procedure, performed at diagnosis and with appropriate controls, is a clinically useful assay in evaluating the risk of tumor recurrence after radical prostatectomy in patients with PAC.</ref><ref>Massimo Cristofanilli,Circulating Tumor Cells, Disease Progression, and Survival in Metastatic Breast Cancer, NEJM Vol 351 august 2004, http://content.nejm.org/cgi/content/abstract/351/8/78</ref>. Often the PCT-technique is used known from the genetic fingerprints. A newer work (december 2007) by Mehmet Toner about an automat registering single cancer cells: <ref>*http://www.istitutoncologicoveneto.it/it/rassegna/2012/201207-02.pdf (nature medicine No 20 december 2007</ref>. Hamer instead believes that there were no studies showing these cancer cells in arterial blood, but this is false and irrelevant because the presence of isolated cancer cells in venous blood of the controlateral side of the tumors can't be explained either. Some articles (out of many) showing cancer cells in arterial blood are: <ref>Yoshihiro Hayata M.D, Significance of Carcinoma Cells in the Blood Relative to Surgery of Pulmonary Carcinoma, Chest 1964;46:51-60.) | ||
| Line 65: | Line 70: | ||
==Handedness== | ==Handedness== | ||
| − | [[image:handedness.jpg|600px|thumb| | + | [[image:handedness.jpg|600px|thumb|Applause-test for handedness according to Hamer]] |
| − | In new medicine, handedness is important as it | + | In new medicine, handedness is important as it is believed to determine the location of an eventual disease like cancer. But in relation to handedness in humans, Hamer made many erroneous statements in obvious contrast to actual medical knowledge. |
| − | *''' | + | *'''Monozygotic twins and handness''': Hamer is convinced that, in monozygotic twins, one was always left-handed while the other one was right-handed, but gives no exact reference for this opinion.<ref>[...] Interessant ist in dem Zusammenhang auch, daß bei eineiigen Zwillingen stets einer linkshändig und der andere rechtshändig ist [...] (from: http://www.neue-medizin.de/html/handigkeit.html)</ref><ref>Hamer RG: Vermächtnis einer Neuen Medizin. Teil 2. Die 5 Biologischen Gesetze - Grundlage der gesamten Medizin.. 7. Aufl. Amici di Dirk - Ediciones de la Nueva Medicina S.L., E-Fuengirola 1999 ISBN 84-930091-0-5</ref> This opinion can easily be checked and there is scientific literature dealing with this issue. Incidence of left-handedness in singletons, monozygotic, and dizygotic twins is around 10%-15%, and there is no source stating that left-handedness was exactly 50% in monozygotic twins.<ref>Derom, Handedness in twins according to zygosity and chorion type: a preliminary report Behav genet 1996 Jul;26(4):407<br> |
In the course of the East Flanders Prospective Twin Survey (EFPTS), handedness was assessed as part of a genealogical study (Meulemans et al., 1995) in 1616 twins (808 twin pairs) aged 6 to 28. Our findings are that, in this large population-based study with known placentation and zygosity, the often observed higher frequency of left-handedness in twins is confirmed, that it appears to be independent of zygosity and chorion type, and that the belief that discordant handedness in monozygotic twins represents mirror-imaging is mythical.</ref> The autor Derom writes: ''[...] the belief that discordant handedness in monozygotic twins represents mirror-imaging is mythical [...]''.<ref>Shimizu A, Comparison of patterns of handedness between twins and singletons in Japan, Cortex 1983 Sep;19(3):345-52<br> | In the course of the East Flanders Prospective Twin Survey (EFPTS), handedness was assessed as part of a genealogical study (Meulemans et al., 1995) in 1616 twins (808 twin pairs) aged 6 to 28. Our findings are that, in this large population-based study with known placentation and zygosity, the often observed higher frequency of left-handedness in twins is confirmed, that it appears to be independent of zygosity and chorion type, and that the belief that discordant handedness in monozygotic twins represents mirror-imaging is mythical.</ref> The autor Derom writes: ''[...] the belief that discordant handedness in monozygotic twins represents mirror-imaging is mythical [...]''.<ref>Shimizu A, Comparison of patterns of handedness between twins and singletons in Japan, Cortex 1983 Sep;19(3):345-52<br> | ||
The handedness questionnaire of thirteen items which was identical to that employed in our previous study on singletons was administered to 62 monozygotic (MZ) and 48 dizygotic (DZ) twin pairs in Japan. Information on forced conversion of hand usage in childhood was also obtained. Results indicated that the incidence of left-handedness was 3.6% and that of non-right-handedness (which includes mixed- and left-handedness) was 5.9%. There was no significant difference in the incidence of left-handedness or of non-right-handedness between MZ and DZ twin groups. The proportion of converted right-handedness in MZ twins was slightly higher than in DZ twins. MZ pairs were somewhat more concordant for handedness than DZ pairs. Item analysis indicated that the incidence of individuals who use the left hand for writing and eating was only 0.9% and 1.8%, respectively. A comparison of the results of the present survey on twins with those of our previous one on singletons revealed that the incidence of left-handedness or non-right-handedness in twins is the same as that in singletons. Twins (especially MZ twins) have experienced a forced conversion to right-hand usage more frequently than singletons.</ref> | The handedness questionnaire of thirteen items which was identical to that employed in our previous study on singletons was administered to 62 monozygotic (MZ) and 48 dizygotic (DZ) twin pairs in Japan. Information on forced conversion of hand usage in childhood was also obtained. Results indicated that the incidence of left-handedness was 3.6% and that of non-right-handedness (which includes mixed- and left-handedness) was 5.9%. There was no significant difference in the incidence of left-handedness or of non-right-handedness between MZ and DZ twin groups. The proportion of converted right-handedness in MZ twins was slightly higher than in DZ twins. MZ pairs were somewhat more concordant for handedness than DZ pairs. Item analysis indicated that the incidence of individuals who use the left hand for writing and eating was only 0.9% and 1.8%, respectively. A comparison of the results of the present survey on twins with those of our previous one on singletons revealed that the incidence of left-handedness or non-right-handedness in twins is the same as that in singletons. Twins (especially MZ twins) have experienced a forced conversion to right-hand usage more frequently than singletons.</ref> | ||
| − | *'''Hamerian | + | *'''Hamerian Applause Test and Prayer Test'''. Hamer uses his own and controversial test for handedness, the so-called ''Applause test'' and a so-called ''Bet-Test'' (prayer test). These simple tests have never been scientifically validated and are of pseudoscientific character. No information regarding these tests can be found in scientific databases. Using these tests, some New Medicine patients were attributed a conflicting handedness by different persons, creating some confusion. |
| − | *'''Handedness and body side to cradle babies'''. Hamer is convinced that women and men | + | *'''Handedness and body side to cradle babies'''. Hamer is convinced that women and men will always cradle their babies on the opposite side of their dominant hand. A left-handed woman thus was to hold the baby on the right side of her body. This is not true, and many scientific sources tell us something different. Men and women hold their baby mostly (80%) on their left side, regardless of handedness. This is also true for apes (primates). <ref>Salk L, The effects of the normal heartbeat sound on the behavior of the new-born infant: implications for mental health. World Mental Health 1960 12, 168-175</ref><ref>De Chateau, Left-side preference for holding and carrying newborn infants. Parental holding and carrying during the first week of life, J Nerv Ment Dis 1983 Apr;171(4):241-5,Four groups of adults were studied: new mothers, new fathers, fathers with older children, and males without children of their own. Nearly 80 per cent of all newly delivered mothers and fathers held their newborn infant against a point to the left of the body midline. Handedness and parity did not influence this preference, nor did the sex of the infant. The present study also demonstrates that new fathers during the neonatal period, as well as fathers with older infants, display a significantly greater preference for holding the infant to the left than males without own children and with or without experience of other children. Individual mother-father pairs held the infant on the same side of the body in the majority of couples studied. The pattern of infant-carrying showed no significant in-between group differences. The possible significance of these observations and their relation to other parental behavior are discussed.</ref><ref>Mason Giorgia, Why do humans and apes cradle babies on their left side? New Scientist, 21. July 1990, 28.</ref><ref>Sieratzki JS, Neuropsychological and neuropsychiatric perspectives on maternal cradling preferences, Epidemiol Psychiatr Soc 2002 Jul-Sep;11(3):170-6 |
OBJECTIVE: To assess competing explanations for the universal preference of mothers to cradle infants on their left side and to propose a relation to hemispheric asymmetry for social attachment and communication behaviour. METHODS: A review of observational, experimental, physiological, psychological, neuro-physiological, and neuro-psychological studies, including new findings on the cradling behaviour of mothers with auditory or visual impairments. RESULTS: A significant left-cradling bias is observed in both right- and left-handed mothers which cannot adequately be explained by arguments based on handedness or closer contact to the soothing sound of the maternal heartbeat. Observations of primate behaviour have led to the suggestion that the left-cradling bias may be related to a left visual field (right hemisphere) advantage for monitoring an infant's facial expressions of distress. However, more than just monitoring, cradling subserves the mother's connection with the infant. For that reason, we have suggested that left cradling might be related to a right hemisphere specialisation for emotional communication, i.e. the speech melody, smiles, signals, and stroking which mothers use to interact with their infants. Studies of mother-infant interaction show that the sound of the mother's voice is more soothing when cradling on the left, more stimulating when cradling on the right. Cradling laterality may thus be related to emotional state and behavioural intent. There is also evidence to suggest that left cradling is linked to a special role of the right hemisphere in social attachment behaviour. This function may be disturbed in mothers with post-natal depression who show abnormal right hemisphere activity. CONCLUSION: Cradling embodies the symbiotic relationship between mother and infant; various lines of evidence support the suggestion that the universal preference of mothers to cradle infants on their left side is related to a right hemisphere dominance for social attachment and communication behaviour.</ref><ref>Bogren LY, Side preference in women and men when holding their newborn child: psychological background, Acta Psychiatr Scand 1984 Jan;69(1):13-23 | OBJECTIVE: To assess competing explanations for the universal preference of mothers to cradle infants on their left side and to propose a relation to hemispheric asymmetry for social attachment and communication behaviour. METHODS: A review of observational, experimental, physiological, psychological, neuro-physiological, and neuro-psychological studies, including new findings on the cradling behaviour of mothers with auditory or visual impairments. RESULTS: A significant left-cradling bias is observed in both right- and left-handed mothers which cannot adequately be explained by arguments based on handedness or closer contact to the soothing sound of the maternal heartbeat. Observations of primate behaviour have led to the suggestion that the left-cradling bias may be related to a left visual field (right hemisphere) advantage for monitoring an infant's facial expressions of distress. However, more than just monitoring, cradling subserves the mother's connection with the infant. For that reason, we have suggested that left cradling might be related to a right hemisphere specialisation for emotional communication, i.e. the speech melody, smiles, signals, and stroking which mothers use to interact with their infants. Studies of mother-infant interaction show that the sound of the mother's voice is more soothing when cradling on the left, more stimulating when cradling on the right. Cradling laterality may thus be related to emotional state and behavioural intent. There is also evidence to suggest that left cradling is linked to a special role of the right hemisphere in social attachment behaviour. This function may be disturbed in mothers with post-natal depression who show abnormal right hemisphere activity. CONCLUSION: Cradling embodies the symbiotic relationship between mother and infant; various lines of evidence support the suggestion that the universal preference of mothers to cradle infants on their left side is related to a right hemisphere dominance for social attachment and communication behaviour.</ref><ref>Bogren LY, Side preference in women and men when holding their newborn child: psychological background, Acta Psychiatr Scand 1984 Jan;69(1):13-23 | ||
In a prospective study 81 randomly selected parents awaiting their first baby were interviewed early during pregnancy and again during the week after delivery. About 80% of the women and their partners were found to hold their child to the left, and 20% to the right, irrespective of handedness. There was no relation between side preference in child holding in the couples. Common to both sexes is the trend that left-holders are more attached to and identified with the parent of their own sex whereas right-holders are more attached to and identified with the parent of the opposite sex. Right-holders have also more often had mental symptoms prior to pregnancy and were concerned about the pregnancy, delivery and health of the child at birth.</ref><ref>Bogren LY, The couvade syndrome and side preference in child holding, Acta Psychiatr Scand 1985 Mar;71(3):311-4,In a prospective study of expectant couples 20% of the men suffered from the couvade syndrome. About 80% of both women and men hold their newborn infant to the left and 20% to the right, irrespective of handedness. Compared with others, men with the syndrome more frequently developed a right-side preference in child holding. Right-holding men more often had sons than daughters. Right-holders with the couvade syndrome were more often attached to and more closely identified with their mothers than were right-holding non-sufferers.</ref><ref>Ginsburg HJ, Maternal holding preferences: a consequence of newborn head-turning response, Child Dev 1979 Mar;50(1):280-1, | In a prospective study 81 randomly selected parents awaiting their first baby were interviewed early during pregnancy and again during the week after delivery. About 80% of the women and their partners were found to hold their child to the left, and 20% to the right, irrespective of handedness. There was no relation between side preference in child holding in the couples. Common to both sexes is the trend that left-holders are more attached to and identified with the parent of their own sex whereas right-holders are more attached to and identified with the parent of the opposite sex. Right-holders have also more often had mental symptoms prior to pregnancy and were concerned about the pregnancy, delivery and health of the child at birth.</ref><ref>Bogren LY, The couvade syndrome and side preference in child holding, Acta Psychiatr Scand 1985 Mar;71(3):311-4,In a prospective study of expectant couples 20% of the men suffered from the couvade syndrome. About 80% of both women and men hold their newborn infant to the left and 20% to the right, irrespective of handedness. Compared with others, men with the syndrome more frequently developed a right-side preference in child holding. Right-holding men more often had sons than daughters. Right-holders with the couvade syndrome were more often attached to and more closely identified with their mothers than were right-holding non-sufferers.</ref><ref>Ginsburg HJ, Maternal holding preferences: a consequence of newborn head-turning response, Child Dev 1979 Mar;50(1):280-1, | ||
| Line 110: | Line 115: | ||
==Invention of the New Medicine in 1981== | ==Invention of the New Medicine in 1981== | ||
| − | Some time after the death of his son Dirk | + | Some time after the death of his son Dirk (see his [[Ryke Geerd Hamer|biography]]), Hamer began to believe that any disease, most notably cancer, was not dangerous in itself, but merely a biological symptom of a psychological conflict situation which he calls biological conflict. The loss of his son led Hamer to invent his "New Medicine" in autumn 1981, while living in Germany. According to Hamer, the shock of his son's death caused him to develop testicular cancer within two months after the event and also caused breast cancer in his wife Sigrid. Being his first patient and refusing any conventional cure by modern medicine, the only medical treatment she received was by R.G. Hamer. Sigrid Hamer died of cancer in 1985. |
==See also== | ==See also== | ||
*[[Victims of New Medicine]] | *[[Victims of New Medicine]] | ||
*[[Testimonies of former associates of Hamer]] | *[[Testimonies of former associates of Hamer]] | ||
| + | |||
| + | {{OtherLang|ge=Germanische Neue Medizin|en=Germanic New Medicine|fr=Nouvelle Médecine Germanique|it=Nuova Medicina Germanica}} | ||
==References== | ==References== | ||
Latest revision as of 23:22, 10 March 2013
Germanic New Medicine® (GNM) (formerly called New Medicine and often called New German[ic] Medicine) is a pseudoscientific, alternative medicine which appeared in Germany in 1981. It is also a registered trade mark since 2003. Many hopeful cancer patients treated by this method have died, at least 140 (see details below).
Germanic New Medicine was invented by barred German physician Ryke Geerd Hamer, who has been prosecuted in several European countries for practicing medicine illegally. Hamer is currently living in Sandefjord, in the south of Norway. His address is the same as his publishing company GERMANISCHE NEUE MEDIZIN FORLAG DR. HAMER Sandkollveien 11, N-3229 Sandefjord/Norway. In two interviews in September 2007, Hamer stated that he fled from Spain to Norway to escape an arrest warrant from Germany. The warrant was issued on grounds of incitement of hatred (article 130 of German criminal law), because of Hamer's many public anti-semitic statements in open letters and on web pages, accusing an alleged international Jewish conspiracy (in particular the New York B'nai B'rith) of having killed two billion people by hiding the truth about New Medicine, which Hamer claims can heal 98% of all cancer cases.
Since its principles are incompatible with the findings of modern evidence-based medicine, GNM has never been accepted and is widely ignored by the scientific and academic medical community. Hamer spreads his ideas in his books, published by his own publishing company Amici di Dirk, via many different private web pages on the internet and through publications by a number of followers and associations supporting his doctrines.
According to Hamer, every disease of either man, animal or plant was the result of an earlier - not well-defined - biological conflict, obeying to no more than five so-called biological laws of nature which he claims to have discovered, but which no scientist has been able to confirm as of yet. In addition to this, Hamer states that only the effects of radiation and injuries were not the result of a biological conflict.
GNM is a mainly diagnostic construction and may be seen as a primitive reinvention of some obsolete concepts of psychosomatic medicine, mixed with pseudoscientific, unvalidated tests of Hamer's own invention and a grotesquely erroneous interpretation of CT brain scans. Some of his ideas have already been proposed before (e.g. Christian Science and anthroposophic medicine etc.). What is usually called disease or symptom, Hamer considers a sensible biological program (in German: sinnvolles biologisches Sonderprogramm), being the reaction of a healthy organism to alleged biological conflicts. According to Hamer's theory, all severe diseases, such as cancer, can be healed in 95% of all cases by performing a so-called conflictolysis according to GNM. Failures of his method or the death of patients are consistently attributed to interventions of scholastic medicine, the use of morphine, or the patient's not being totally committed to GNM.
Hamer does not present any literature supporting his ideas; some of his assertions, however, remind of concepts to be found in anthroposophical medicine and other concepts developed earlier than 1981. No prospective and scientifically controlled clinical test has been made so far to prove a possible efficacy, and no peer-reviewed articles in serious medical journals exist.
Germanic
Germanic is a term which first appeared in Roman times about 200 years before Christ and was used by Romans (for instance Pliny the elder) to designate different peoples living east of the Rhine river or north of the Alps. These different peoples never called themselves Germanic. This term was an invention of some of the enemies of the different Germanic peoples and tribes. When, in 2004, Hamer was asked why he wanted his hypotheses to be called Germanic, he answered: [...] weil ich stolz bin ein Deutscher zu sein [...] (because I'm proud to be a German).[1] Hamer also justified the term in his book Vermächtnis einer neuen Medizin[2], asserting that the term Germanic allegedly carried no concept of evil or good as this allegedly only appeared in Judaic and Christian tradition. Hamer also expressed his conviction that medicine had been invented in Germany, the country of poets, musicians, inventors and discoverers, and that Germany was the mother of all European languages, which is nonsense.
No published reports about healed cancer patients so far
No report about healed cancer patients who survived a GNM therapy and who were not treated by academic medicine has been published so far, only some anecdotal stories are available. For instance a German person asserts that he survived leukemia eleven times thanks to Hamer's method,[3] another person asserts to have been healed miraculously from an atheroma (this is not cancer), and someone thinks that his torticollis was in fact a non-Hodgkin lymphoma[4]. Admirers and followers of GNM believe that thousands of cancer patients have been healed by GNM. A neutral observer must wonder why they do not show up to support this method.
Notable cases of failure
Many former GNM patients suffering from cancer died. More than 140 persons were known as of 2008. This is documented in different court files and sentences, newspaper articles, reports of relatives, and in the list presented by Aribert Deckers.[5] Many of them had a good chance to survive as they had a cancer responding well to modern therapies (e.g. testicular cancer, Hodgkin-lymphoma). A detailed presentation of notable cases can be seen here: Victims of New Medicine.
Ryke Geerd Hamer developed testicular cancer himself in 1978 (or at the beginning of 1979), but seeked professional help and underwent surgery in a clinic in Tübingen. He survived this miraculously, according to his own opinion he should have had a survival chance of only 2%.[6] His tumor appeared only two months after the death of his son Dirk (which was in December 1978), and Hamer was convinced of this event being the cause of his cancer.[7]. But cancer needs years to develop, and not two months. His wife died from breast cancer in 1985, a GNM therapy by Hamer was not successful. Hamer said this at the end of 1985 and declared his wife to be his first patient after discovering the iron rules of cancer.
Sceptical view of GNM
Hamer never published his hypotheses in a scientific paper (his doctoral thesis has nothing to do with it), and apart from an article by Danish holistic physician (now barred) Sören Ventegodt which appeared in a rather unimportant journal[8], no scientific paper analysing his method can be found in databases. The author Ventegodt also lost his medical licence in the meantime and has been criticized for working in a pseudoscientific way; furthermore the journal apparently accepts papers after receiving a payment.[9] This makes it more difficult to evaluate his ideas.
Hamer does not present scientific proof in favour of his method, and does not present controlled and placebo-controlled prospective studies supporting it. Instead, he shows retrospectively filtered reports and letters of anecdotal value, often written by himself or laypersons.
Hamer does never recognise any limit of his medical knowledge (he could not work as physician after 1986) and behaves as an expert in every branch of medicine, exactly as described by the Dunning-Kruger effect[10][11], becoming a danger to his patients.
External and Internal Contradictions and Obvious Errors
Many of Hamer's different public statements regarding his doctrines are in conflict with each other and in a clear contrast and conflict to the actual knowledge in scientific medicine.
- Cancer: Hamer states that he was able to cure cancer patients in 98% of all cases but is unable to present a single cured patient. At the same time, it is well known (see his trials, the Aribert-Decker-List[12] and Victims of New Medicine / Testimonies of former associates of Hamer) that many cancer patients following his method died. Some of his statements seem to indicate that the therapeutic principle in new medicine is the so far unknown induction of a spontaneous remission of cancer after a psychotherapeutical intervention by the patient himself, and assisted by a GNM therapist. The probability of any spontaneous remission, however, is known to be very low, occuring only in about 1:50,000 to 1:140,000 of all cancer cases. These remissions are not only very rare, but at the same time no cure is known today to induce them. Every spontaneous remission is also subject to possible relapses and patients must wait at least five (or more) years until they know that recovery seems to be definitive. At least two different groups of experts are performing research on spontaneous remissions in Germany (one for instance in Nuremberg). At the same time, Hamer declared many times, and still continues to repeat, that scientific medicine offered only about a 2% survival chance for a cancer patient.[13] Hamer sometimes refers to Ulrich Abel, a German expert who never made any statement like this. In reality, modern medicine (evidenced-based medicine and good clinical practice) today offers a survival rate of about 55% (all cases) in Germany[14], and in other countries, like the USA or Australia, even over 60%[15]. National Cancer Institute (USA) indicates a cancer survival of only 20% in 1920. And cancer incidence started to decrease about ten years ago in Germany.[16]
- Another big error: Hamer claims that 1,500 German non-Jewish cancer patients were killed every day by scientific medicine and this can be seen or heard in a video interview dated 2006[17] and he continues to assert this claim on different web pages in open letters.[18] These data, however, contradict published German cancer statistics of 2002: 420,000 people were newly diagnosed with cancer in that year in Germany, and at the same time 210,000 died because of cancer in 2002. 210000/365=575, Hamer's numbers cannot be correct and 1,500 x 365 = 547,500. This means the number of dead patients would exceed the number of newly diagnosed patients by 120,000. This is of course impossible.
- Chemotherapy and cancer: According to Hamer, chemotherapy in cancer treatment would have a fatal effect on every patient and caused the death of many people in the past. However, chemotherapy is mostly used as a coadjuvant therapy combined with surgery or a radiation therapy. Some (not all) cancers are sensitive to particular drugs used. Cancer of this type for instance is Acute Lymphoblastic Leukemia in children, Hodgkin-disease or testicular cancer.[19]. Overall (additional = contribution for chemotherapy for cancer survival is estimated at between 5-10%.
- Tumors in transplanted organs: Tumors may also come up in transplanted organs, they were already present in these organs before transplantation (too small to be detected), but it is also known that a tumor can build up after transplantation. After a transplantation, no nerve links this organ to the brain, and therefore the GNM theory of cancer origin fails.[20][21][22][23][24][25][26]
- Inherited cancer: In some cancer types it is known for sure that these are inherited and therefore transmitted genetically. One example is familial adenomatous polyposis[27] or Xeroderma pigmentosum[28]. Other cases are Louis-Bar syndrome, Gardner syndrome, Turcot syndrome and familiar form of retinoblastoma. In these cases a biological conflict as an origin can be excluded.
- Cancer caused by virus: About 15% of all cancer are caused by viruses (oncovirus), the presence of a viral infection increases incidence. This is the case in high-risk HPV, Burkitt lymphoma and HIV.
- No chemical carcinogens in new medicine: The Hamer doctrine allows no chemical carcinogens to exist, they have simply no effect on tumour formation and smoking does not cause cancer, for instance. Cancer may occur because people were in panic after hearing that carcinogens like asbestos were harmful.
- No metastasis in GNM: According to the same doctrine metastases do not exist and allegedly were never proved by scientific medicine. Tumours appearing after a first tumour were due to the panic of the patient who, suffering, was producing new tumours. Also, isolate tumor cells would not be detectable in blood, especially not in arterial blood.[29] Many scientific articles tell us the opposite. Since 1869 (more than 130 years ago), it is known that tumors emit single cancer cells or groups of them into the blood, and every day a tumor may emit millions of cells even if only a minority may survive (perhaps 0,01%) and be the source of a distant metastasis[30][31][32][33][34][35][36][37][38][39][40][41]. Often the PCT-technique is used known from the genetic fingerprints. A newer work (december 2007) by Mehmet Toner about an automat registering single cancer cells: [42]. Hamer instead believes that there were no studies showing these cancer cells in arterial blood, but this is false and irrelevant because the presence of isolated cancer cells in venous blood of the controlateral side of the tumors can't be explained either. Some articles (out of many) showing cancer cells in arterial blood are: [43], Yamaguchi [44] and Georgakoudi [45]. See also: [46]. Isolated cancer cells were also found in sputus, urine, sperma and stool [47]). Arterial-venous shunts did not influence metastasis formation: [48], and cancer cells can move from the blood into tissue: [49], [50] and the number of circulating cancells is correlated positively with the probability of metastasis formation. In some particular cancer the metastasis formation is well known and obvious (Krukenberg cancer).
- No brain tumors in New Nedicine: brain tumors simply do not exist in New Medicine, the theory eliminates them by definition. It was argued that nervous cells were not able to divide. Nobel price for Rita Levy-Montalcini (nerve growth factor) proves the opposite and so do scientific studies [51][52][53]. Many different brain tumor develop also out of glial cells or other cells in the brain that are not neurons. The existence of brain tumors would disturb the iron rule in new medicine, that a conflict creates a so-calles DHS and determines a tumor in a brain-depending and handedness-depending organ.
- Transmissible cancer in animals: in some animals, transmissible cancer can be found. This is of course not compatible with New Medicine doctrine. Some example are: CTVT in dogs [54] [55][56], DFTD in Tasmania [57], and tumors riginating out of particular proteins of JSRV [58]. Work of Tanaka (1990) shows the experimental transmision of cancer from a mouse to another mouse: [59].
Role of morphine in New Medicine
Morphine (derived from opium) was invented about 200 years ago in 1804 by Friedrich Wilhelm Sertürner, after opium had been used for thousands of years. Morphine allowed a more exact dosage in pain relieving treatment. Hamer and his followers are convinced that the use of morphine (and similar drugs) were the cause of many cancer deaths. Morphine, however, is one of the most powerful analgetic drugs we know today and has no ceiling effect. Morphine can be easely dosed by a patient adding only the necessary number of drops to a beverage. Its side effects must be known by each medical student and they are well known since the invention in 1804. In Denmark, morphine consumption in the 80ies was known to be ten times higher than in Germany, without influencing cancer mortality (75 kg/1 milion persons/year instead of 7,5 kg), and in 2002, morphine consumption increased to 22 chili in Germania, while cancer mortality was decreasing. In Italy, consumption was 70 kg, 92 Kg in Denmark, in Austria 152 kg, UK 353 Kg and Hungary 577 Kg/1 mil./year.
Role of Pain
Pain, Hamer believes, should not be treated (see: Testimonies of former associates of Hamer). According to protagonists of the method, no opiates or opiate derivates should be administered as far as possible if chances for a cure are not to be practically eliminated. This can cause patients to endure extreme cancer pain unnecessarily on the assumption this was necessary for a cure (see: Victims of New Medicine). Moreover, if the cancer progresses, patients could suffer feelings of failure or guilt, because the Hamer method of «New Medicine» presumes that the cure for cancer depends upon the patients’ resolving their personal conflicts. This could give rise to the erroneous assumption that the disease will progress if they do not make a large enough contribution towards the resolution of their conflicts, or if they do not follow the proper procedure.
Handedness
In new medicine, handedness is important as it is believed to determine the location of an eventual disease like cancer. But in relation to handedness in humans, Hamer made many erroneous statements in obvious contrast to actual medical knowledge.
- Monozygotic twins and handness: Hamer is convinced that, in monozygotic twins, one was always left-handed while the other one was right-handed, but gives no exact reference for this opinion.[60][61] This opinion can easily be checked and there is scientific literature dealing with this issue. Incidence of left-handedness in singletons, monozygotic, and dizygotic twins is around 10%-15%, and there is no source stating that left-handedness was exactly 50% in monozygotic twins.[62] The autor Derom writes: [...] the belief that discordant handedness in monozygotic twins represents mirror-imaging is mythical [...].[63]
- Hamerian Applause Test and Prayer Test. Hamer uses his own and controversial test for handedness, the so-called Applause test and a so-called Bet-Test (prayer test). These simple tests have never been scientifically validated and are of pseudoscientific character. No information regarding these tests can be found in scientific databases. Using these tests, some New Medicine patients were attributed a conflicting handedness by different persons, creating some confusion.
- Handedness and body side to cradle babies. Hamer is convinced that women and men will always cradle their babies on the opposite side of their dominant hand. A left-handed woman thus was to hold the baby on the right side of her body. This is not true, and many scientific sources tell us something different. Men and women hold their baby mostly (80%) on their left side, regardless of handedness. This is also true for apes (primates). [64][65][66][67][68][69][70][71][72][73][74][75] [76][77].
Handedness was an object of research for a long time and is detected by particularly complex tests developed during the 1940ies, taking into account cultural influences [78][79][80][81][82][83][84][85][86]
Hamer and Radiology
See also: Hamer-Focus article
Hamer bases his diagnoses on a particular interpretation of brain scans using exclusively computer tomography mixed with his obscure and never validated proprietary handedness tests. CT-diagnostics is crucial in New Medicine to detect so-called Hamer foci. His particular interpretation is not compatible with actual knowledge in radiology. The Swiss Study Group for Complementary and Alternative Methods in Cancer writes: [...] The «Hamer foci» on the CT images in Hamer׳s books have been identified by radiological experts as typical artefacts produced by the radiological device which can appear in a poor-quality CT scan [...][87] and the author Ventegodt adds: [...] The concentric circles in the Hamer focus, shown on the front page of his book[1], looks like an artefact and very little as a biological phenomena, which in humans are almost never seen as concentric circles [...].[88]
Hamer believes that a sudden shock-like onset of unforeseen (and overwhelming) emotional conflicts experienced alone would lead to a Dirk-Hamer-Syndrome (DHS), which immediately, within a fraction of a second, produces a «cancer or cancer equivalent in an organ». He postulates that every emotional process will take place synchronously in the brain, in the «organic brain» and in the organ. He adds that the tumours are allegedly controlled by the part of the brain that is ontogenetically connected with the organ in question. Hamer calls this the «ontogenetic system of tumours». In the brain, the so-called biological conflict is said to give rise to the development of a Hamer focus. By this, Hamer means particular configurations in CT brain scans which are shaped like a shooting target, and that had never been seen by radiologists before, the non-radiologist Hamer adds. He claims that the locations of the Hamer foci and their degree of severity correlate to the organs affected, the underlying biological conflict, and the phase of the conflict.
Many brain-scans presented by Hamer in his books and elsewhere, clearly show well-known ring-artefacts in radiology. Some of theses ring-artifacts can be seen on the front page of Hamer's books, and on the front page of other publications of his followers.
Professor Maximilian Reiser (university of Munich) and president of German radiologists (Deutsche Röntgengesellschaft) was presented with some CT brain-scans taken from a book of Hamer's.[89] Reiser wrote in an expert opinion the day 22, January, 2007: [90]
expert opinion of Prof. Dr. med. Dr. h.c. Maximilian Reiser, Director of the Institute of Radiology for Clinical Radiology of the Ludwig-Maximilian-University Munich, President of Deutsche Röntgengesellschaft.
I confirm that the brain-scans presented in the "work" of Mr. Hamer have been interpreted in a completely inappropriate way by the author and are in clear conflict to scientifically justified knowledge and experience. An argumentative discussion with the content of Hamer's theories and the related interpretations of the brain scans in my opinion is not possible or goal-leading because Mr. Hamer is moving in a hermetically closed ambience of ideas and refuses any criticism as the expression of an arrogant "scientific medicine". I would like to confirm your corrections made in respect of some CT findings.
You may of course quote this opinion as the opinion of the President of "Deutsche Röntgengesellschaft"
Sincerely, M. Reiser"
A single CT-scan produces a dose of radiation. A single CT brain-scan corresponds to about 4 mSv and corresponds approximately to the annual dose of radiation a person receives from any other source (natural and man-made).
Invention of the New Medicine in 1981
Some time after the death of his son Dirk (see his biography), Hamer began to believe that any disease, most notably cancer, was not dangerous in itself, but merely a biological symptom of a psychological conflict situation which he calls biological conflict. The loss of his son led Hamer to invent his "New Medicine" in autumn 1981, while living in Germany. According to Hamer, the shock of his son's death caused him to develop testicular cancer within two months after the event and also caused breast cancer in his wife Sigrid. Being his first patient and refusing any conventional cure by modern medicine, the only medical treatment she received was by R.G. Hamer. Sigrid Hamer died of cancer in 1985.
See also
Versions of this article in other languages
- Français: Nouvelle Médecine Germanique
- Deutsch: Germanische Neue Medizin
- Italiano: Nuova Medicina Germanica
References
- ↑ Caroline Markolin (Montreal/Canada), January 1, 2005: [...] Ich habe Dr. Hamer letztes Jahr während eines Seminar in Spanien gefragt: "Warum germanisch?". Seine Antwort kam schnell und war eindeutig: "Ich bin stolz, Deutscher zu sein [...] source: http://www.pilhar.com/Hamer/Korrespo/2005/20050101_Markolin_Plaedoyer.htm
- ↑ Hamer RG: book Vermächtnis einer neuen Medizin chapter 28
- ↑ case Joswig, a German extremist right admirer of GNM who claims to be a citizen of Deutsches Reich (German empire)
- ↑ http://www.pilhar.com/Hamer/NeuMed/Sonderpr/20000101_NonHodgkin.htm
- ↑ http://www.ariplex.com/ama/ama_ham2.htm
- ↑ http://www.neue-medizin.de/html/ein_vermachtnis.html
- ↑ http://www.newmedicine.ca/interview.php [...] in 1978 I developed testicular cancer from such a biological conflict, a so-called "loss conflict [...]"
- ↑ Ventegodt et al. Fulltext: http://www.thescientificworldjournal.com/headeradmin/upload/2005.03.16.pdf
- ↑ http://kasperolsen.wordpress.com/2005/12/19/more-dangerous-pseudo-science/ Ventegodt and pseudoscience
- ↑ Justin Kruger, David Dunning (1999), "Unskilled and Unaware of It: How Difficulties in Recognizing One's Own Incompetence Lead to Inflated Self-Assessments". Journal of Personality and Social Psychology 77 (6): 1121–34. PMID 10626367. [1]
- ↑ http://en.wikipedia.org/wiki/Dunning-Kruger_effect
- ↑ http://www.ariplex.com/ama/ama_ham2.htm
- ↑ [...] So aber gibt es nur schlechte Verlierer in der dummen und falschen Schulmedizin. Von der strafrechtlichen Seite wollen wir noch gar nicht einmal sprechen., d.h. von der Frage, wer denn für den seit 18 Jahren geübten, vorsätzlichen wissenschaftlichen Massenmord oder Superholokaust an unseren Patienten verantwortlich ist. Denn beim Deutschen Krebsforschungszentrum Heidelberg kann sich doch jeder erkundigen: Bei der "Standesamtsstatistik" (d.h.: Wer lebt wirklich noch nach Chemo-Pseudotherapie ?) findet man, daß nach 5 Jahren 95% der Patienten tot sind, nach 7 Jahren 98%! Das heißt: Man hat alle Patienten regelrecht um ihr Leben betrogen, indem man die Erkenntnisse der neuen Medizin mit ihrer 95%igen (und mehr) Überlebenschance unterdrückt hat! Das war aber nicht ein paar vertrottelte Medizyn-Onkelchens oder saudumme Medienredakteure, xxxxx Richter oder Politiker, sondern das waren die finsteren Mächte der Logenonkelchen und Onkologenbrüderchen, die dieses schlimmste Verbrechen der Menschheitsgeschichte für den Wahn der Weltherrschaft begehen mußten [...] see: http://www.pilhar.com/Hamer/Korrespo/1999/19990415_Hamer_an_Freund_Gallmeier.htm (rif 107)
- ↑ Robert Koch Institut, Germany
- ↑ http://annonc.oxfordjournals.org/cgi/reprint/14/suppl_5/v61.pdf (periodo 1990-94, pag. 58)
- ↑ http://www.aerzteblatt.de/v4/archiv/bild.asp?id=12796 (source: http://www.ekr.med.uni-erlangen.de/GEKID/Doc/kid2006.pdf)
- ↑ http://www.lnc-2010.de/html/neues_deutschland.html
- ↑ http://www.pilhar.com/Hamer/Korrespo/2007/20070205_Hamer_an_HR3.htm
- ↑ Brandt L, A systematic overview of chemotherapy effects in Hodgkin's disease, Acta oncol 2001;40(2-3):185-97, A systematic review of chemotherapy trials in several tumour types was performed by The Swedish Council of Technology Assessment in Health Care (SBU). The procedures for the evaluation of scientific literature are described separately (Acta Oncol 2001; 40: 155-65). This synthesis of the literature on chemotherapy for Hodgkin's disease (HD) is based on 113 scientific reports including four meta-analyses, 44 randomised studies, 18 prospective studies and 40 retrospective studies. These studies involve 69,196 patients. The conclusions reached can be summarised into the following points: Chemotherapy is of utmost importance for the cure of HD. At early stages, extended field radiotherapy cures most patients. For the majority of patients with relapses after radiotherapy, chemotherapy is curative and the total proportion of cured early stage patients is 75-90%. Chemotherapy in addition to extended field radiotherapy reduces recurrences but does not improve long-term survival. In early stage HD with a large mediastinal mass and/or systemic symptoms, combined treatment with chemotherapy and radiotherapy is recommended. It is likely that chemotherapy will in future play a greater role in the treatment of early stage patients, too, in order to reduce later consequences from extended field radiotherapy. However, this conclusion remains to be better documented in literature. At advanced stages, chemotherapy or a combination of chemotherapy and limited field radiotherapy are effective treatment options and, using the regimens available 10-20 years ago, 40-50% of the patients are cured. Based upon more favourable short-term (three to eight years) results of more recently developed regimens, it can be expected that today a higher proportion of the patients will become long-term survivors. Several chemotherapy regimens containing four to eight drugs are effective in HD. The best regimen considering both antitumour activity and acute and later side-effects is not known. The choice of regimen is probably best done after considering various pre-treatment factors such as the number of poor prognostic signs, concomitant diseases, and individual preferences. The results of chemotherapy are more favourable in young than in elderly patients. The development of less toxic but still effective treatment programmes is therefore particularly important for the elderly. High dose chemotherapy with stem cell support is presently often used in patients who are chemotherapy induction failures, who relapse after a short initial remission or after a longer initial remission and treated initially with seven or eight drugs, or who have had multiple relapses. However, this use is based on data from uncontrolled or small controlled studies, not being fully convincing with respect to effect on survival. Persistent side-effects of treatment are common among long-term survivors, although most patients apparently have a normal life. The relative contributions of chemotherapy and radiotherapy to the persistent effects are not well documented.
- ↑ Schwarz A, Renal cell carcinoma in transplant recipients with acquired cystic kidney disease, Clin J Am Soc Nephrol. 2007 Jul;2(4):750-6. Epub 2007 Apr 25 [...] CONCLUSIONS: Renal cell carcinoma occurs often after renal transplantation [...]
- ↑ Aguilera Tubet C, Multifocal renal cell carcinoma on renal allograft, Actas Urol Esp. 2007 May;31(5):553-5 [...] We report a case of multifocal renal cell carcinoma diagnosed in a kidney grafted 17 years before [...]
- ↑ Besarani D Urological malignancy after renal transplantation, BJU Int. 2007 Sep;100(3):502-5
- ↑ Roithmaier S, Incidence of malignancies in heart and/or lung transplant recipients: a single-institution experience, J Heart Lung Transplant. 2007 Aug;26(8):845-9
- ↑ Ondrus D The incidence of tumours in renal transplant recipients with long-term immunosuppressive therapy, Int Urol Nephrol. 1999;31(4):417-22
- ↑ Birkeland SA Risk for tumor and other disease transmission by transplantation: a population-based study of unrecognized malignancies and other diseases in organ donors, Transplantation. 2002 Nov 27;74(10):1409-13
- ↑ Buell JF Donor transmitted malignancies, Ann Transplant. 2004;9(1):53-6
- ↑ http://en.wikipedia.org/wiki/Familial_adenomatous_polyposis
- ↑ http://en.wikipedia.org/wiki/Xeroderma_pigmentosum
- ↑ http://www.neue-medizin.de/html/3__naturgesetz.html
- ↑ Wong LS, Detection of circulating tumour cells and nodal metastasis by reverse transcriptase-polymerase chain reaction technique, Br J surg 2005 Vol 84 (6) 834, In the search for occult metastases in lymph nodes or circulating tumour cells, a reverse transcriptase-polymerase chain reaction (RT-PCR) assay was developed to detect tumour-specific splice variants of the transcript of the CD44 gene. The assay was highly sensitive and could detect ten tumour cell per 10(5) leucocytes. METHODS: RNA was purified from peripheral blood (n = 24) and regional lymph nodes (n = 14) from patients with colorectal cancer. Complementary DNA was made and amplified using primers specific for the CD44 gene. Southern blotting with exon-specific probes was used to enhance the sensitivity. RESULTS: Tumour cells were detected in peripheral blood samples in four patients and lymph nodes in nine, in one of whom conventional histology had not detected tumour cells. CONCLUSION: This technique may be useful in the early diagnosis of primary or metastatic tumours, in assessing prognosis and in detecting residual disease after treatment.
- ↑ Sadahiro S, Detection of Carcinoembryonic Antigen Messenger RNA-Expressing Cells in Peripheral Blood 7 Days After Curative Surgery is a Novel Prognostic Factor in Colorectal Cancer, Ann Surg Oncol 2007 jan 3, BACKGROUND: The significance of detection of circulating cancer cells in blood during surgery in patients with colorectal cancer (CRC) remains controversial. Experimental study revealed that the cancer cells injected from the vein disappeared completely until 7 days. The aim of this study was to clarify that the detection of circulating cancer cells in blood taken later than 7 days after curative surgery may be a prognostic factor. METHODS: Two hundred consecutive patients with CRC who underwent potentially curative surgery were the subjects. Peripheral blood was collected between 7 and 10 days after resection. Cancer cells were detected using reverse transcriptase-polymerase chain reaction targeting carcinoembryonic antigen (CEA) messenger RNA (mRNA). The median follow-up period was 52 months (range: 34-69 months). RESULTS: The overall positive incidence of CEA mRNA was 22%. Detection of CEA mRNA was not significantly related to conventional clinicopathological findings. Recurrence has been confirmed in 55 patients (28%). The recurrence rate was significantly higher in patients with rectal cancer, deep penetration, lymph node metastasis, preoperative chemoradiotherapy and positive CEA mRNA. The CEA mRNA positive patients showed significantly poorer disease free survival (DFS) and overall survival (OS) than the negative patients (DFS, P=0.007; OS, P=0.04). Multivariate analysis revealed that the positive expression of CEA mRNA (P < 0.01) as well as the tumor location and TNM stage classification was identified as the significant risk factors for recurrence. CONCLUSIONS: Detection of CEA mRNA expressing cells in peripheral blood 7 days after curative surgery is a novel independent factor predicting recurrence in patients with CRC.
- ↑ Castells A, Detection of colonic cells in peripheral blood of colorectal cancer patients by means of reverse transcriptase and polymerase chain reaction, Br J Cancer, 1998 78(10) 1368, Circulating tumour cells play a central role in the metastatic process, but little is known about the relationship between this cellular subpopulation and the development of secondary disease. This study was aimed at assessing the presence of colonic cells in peripheral blood of patients with colorectal cancer in different evolutionary stages, by means of reverse transcriptase polymerase chain reaction (RT-PCR) targeted to carcinoembryonic antigen (CEA) mRNA. In vitro sensitivity was established in a recovery experiment by preparing serial colorectal cancer cell dilutions. Thereafter, 95 colorectal cancer patients and a control group including healthy subjects (n = 11), patients with other gastrointestinal neoplasms (n = 11) or inflammatory bowel disease (n = 9) were analysed. Specific cDNA primers for CEA transcripts were used to apply RT-PCR to peripheral blood samples. Tumour cells were detected down to five cells per 10 ml blood, thus indicating a sensitivity limit of approximately one tumour cell per 10(7) white blood cells. CEA mRNA expression was detected in 39 out of 95 colorectal cancer patients (41.1%), there being a significant correlation with the presence of distant metastases at inclusion. None of the healthy volunteers and only 1 of 11 patients (9.1%) with other gastrointestinal neoplasms had detectable CEA mRNA in peripheral blood. By contrast, CEA mRNA was detected in five of the nine patients (55.6%) with inflammatory bowel disease. These results confirm that it is feasible to amplify CEA mRNA in the peripheral blood, its presence being almost certainly derived from circulating malignant cells in colorectal cancer patients. However, CEA mRNA detectable in blood of patients with inflammatory bowel disease suggests the presence of circulating non-neoplastic colonic epithelial cells.
- ↑ Nakamori S, Genetic detection of colorectal cancer cells in circulation and lymph nodes, Dis Colon Rectum 1997 40(10 sup) S29-36, PURPOSE: This study was undertaken to investigate the clinical implications of detection of genetic alterations in blood and lymph nodes in colorectal cancer patients. METHODS: The reverse transcriptase polymerase chain reaction product of the cytokeratin gene in blood was examined as a cancer cell-specific expression in 35 colorectal cancer patients. The K-ras or p53 gene mutations in the lymph nodes histopathologically negative for metastasis were studied by the mutant-allele-specific amplification method in 26 colorectal cancer patients. RESULTS: The reverse transcriptase polymerase chain reaction assay was able to detect a cytokeratin reverse transcriptase polymerase chain reaction product at a concentration from a single to ten colon cancer cells per 10(6) normal peripheral blood mononuclear cells. Cytokeratin reverse transcriptase polymerase chain reaction products were detected in nine patients' blood samples, although none of the samples were cytologically detectable. The blood's cytokeratin positivity correlated with the invasive mode of the tumor (P < 0.05) and the presence of distant metastasis (P < 0.01). Two (50 percent) of four patients whose blood was positive for cytokeratin had recurrences. Of 17 patients with the K-ras or p53 gene mutation in primary tumors, 9 (53 percent) had the corresponding mutations in lymph nodes. Mutation positivity in lymph nodes correlated with the presence of lymphatic invasion of the primary tumor (P < 0.05). All patients with mutation-negative lymph nodes remained disease-free for more than two years after surgery. CONCLUSION: Detection of cytokeratin reverse transcriptase polymerase chain reaction products in the blood and K-ras or p53 gene mutations in the lymph nodes histologically negative for metastasis may be applicable for clinical use, despite some limitations, and may serve as a useful clinical factor for stratifying patients who are at high or low risk for recurrence after surgery.
- ↑ Iinuma H, Detection of tumor cells in blood using CD45 magnetic cell separation followed by nested mutant allele-specific amplification of p53 and K-ras genes in patients with colorectal cancer, Int J Cancer 2000 89(4) 337, A new method for detecting circulating tumor cells that is based on magnetic-activated cell separation (MACS) and nested mutant allele-specific amplification (nested MASA) was evaluated in patients with colorectal cancer using the p53 and K-ras genes as genetic markers. By negative selection with anti-CD45 monoclonal antibody-conjugated supermagnetic microbeads, the proportion of tumor cells was enriched 9-fold. By the combination of MACS and nested MASA, 10 tumor cells in 10(7) normal peripheral blood mononuclear cells could be detected without false-positives. Using this method, we examined blood taken from the tumor drainage veins of 23 patients with colorectal cancer. Eighty-seven percent (20/23) of primary tumor tissues showed p53 and/or K-ras gene mutations. Forty-five percent (9/20) of patients with p53 and/or K-ras mutations in the primary tumor showed the same mutated genes in the blood samples. There was a significant association between the presence of p53 and K-ras gene mutation in the blood and tumor size, depth of invasion, and venous invasion. Blood gene mutation was detected in 80% (4/5) of samples from patients with synchronous liver metastases. Sixty percent (3/5) of patients with mutant genes in the blood developed asynchronous liver metastases after surgery. The overall survival of patients with p53 and/or K-ras gene mutation-positive findings in blood was significantly shorter than that of patients testing negative on Kaplan-Meier analysis. Our results suggest that the method may be useful for reliable detection of tumor cells circulating in the blood and may help to identify patients at high risk for relapse. Copyright 2000 Wiley-Liss, Inc.
- ↑ Wang JY, Molecular detection of APC, K- ras, and p53 mutations in the serum of colorectal cancer patients as circulating biomarkers, World J Surg 2004 28(7) 721, Early detection of tumor DNA in serum/plasma prior to the development of recurrence or metastases could help improve the outcome of patients with colorectal cancer (CRC) after tumor resection. Recent advances in the detection of tumor DNA in the serum/plasma has opened up numerous new areas for investigation and new possibilities for molecular diagnosis. APC and K- ras mutations are considered to be early-stage developments of CRCs, whereas p53 mutations are thought to be relatively late events in the tumorigenesis of CRCs. The aim of this study was to search for the presence of genetic mutations in the DNA extracted from the serum of CRC patients and healthy subjects. We simultaneously evaluate the significance of APC, K- ras, and p53 gene mutations in cancer tissues and their paired serum samples of 104 CRC patients by polymerase chain reaction-single strand conformation polymorphism analysis (PCR-SSCP) followed by direct sequencing. Additionally, analysis was carried out to detect the serum carcinoembryonic antigen (CEA) levels in CRC patients. Overall, we found at least one of the gene mutations in tumor tissues from 75% (78/104) of the CRC patients. Comparison of the three molecular markers showed that the detection rates in the serum were 30.4%, 34.0%, and 34.2% for APC, K- ras, and p53 genes, respectively. Of these patients, 46.2% (36/78) were identified as having positive serum results, whereas all healthy controls remained negative. The overall positive tumor DNA detection rates in the serum were 0% (0/7) for Dukes' A classification, 22.4% (11/49) for Dukes' B, 48.7% (19/39) for Dukes' C, and 66.7% (6/9) for Dukes' D. The detection rate increased as the tumor stage progressed ( p = 0.012). Concurrently, a significant difference was observed between lymph node metastases and positive serum tumor DNA detection ( p < 0.001). A significantly higher postoperative metastasis/recurrence rate in patients harboring gene mutations with serum tumor DNA than those without serum tumor DNA was also demonstrated ( p < 0.001). However, no significant correlation between the postoperative metastasis/recurrence and serum CEA levels was observed ( p = 0.247). These data suggest that the identification of circulating tumor DNA using the molecular detection of APC, K- ras, and p53 gene mutations is a potential tool for early detection of postoperative recurrence/metastases. Moreover, these genes may be potential molecular markers of poor clinical outcome in CRC patients.
- ↑ Wang JY, Molecular detection of circulating tumor cells in the peripheral blood of patients with colorectal cancer using RT-PCR: significance of the prediction of postoperative metastasis, World J Surg 2006 june 30(6) 1007, BACKGROUND: Approximately 20%-45% of colorectal cancer (CRC) patients ultimately develop local recurrence or metastasis following curative surgical resection. The latter is caused by tumor cells shed from the primary carcinoma prior to or during operation, currently undetected by standard clinical staging. Fortunately, the presence of tumor cells in peripheral blood can be detected by molecular methods and is being regarded increasingly as a clinically relevant prognostic factor. MATERIALS AND METHODS: To detect the presence of circulating tumor cells and evaluate their relationship to postoperative metastatic relapse, we simultaneously examined human telomerase reverse transcriptase (hTERT), cytokeratin-19 (CK-19), cytokeratin-20 (CK-20), and carcinoembryonic antigen (CEA) mRNA (messenger RNA) in the peripheral blood of 72 CRC patients and 30 healthy individuals. Using a reverse-transcriptase polymerase chain reaction (RT-PCR), these tumor-related mRNAs were amplified; in addition, analyses were carried out for their correlation with patients' clinicopathologic features, as well as the occurrence of postoperative metastasis. RESULTS: In RT-PCR analysis of the peripheral blood, 69.4% (50 out of 72), 66.7% (48 out of 72), 52.8% (38 out of 72), and 72.2% (52 out of 72) of CRC patients were positive for hTERT, CK-19, CK-20, and CEA mRNA respectively. All 30 healthy individuals were negative for hTERT and CEA mRNA expression, while 2 were positive for either CK-19 mRNA or CK-20 mRNA expression. The detection of CEA mRNA was significantly correlated with depth of tumor invasion (P=0.012), vessel invasion (P=0.035), TNM stage (P<0.0001), and postoperative metastasis (P<0.0001), while positive hTERT mRNA was correlated with TNM stage (P=0.037) and CK-19 was correlated with depth of tumor invasion (P=0.039) and postoperative metastasis (P=0.017). In addition, multivariate logistic regression showed that only CEA mRNA was an independent and significant predictor of postoperative metastasis (P=0.006). Our findings suggest that CEA mRNA may be a more reliable marker than hTERT, CK-19, and CK-20 for the detection of circulating cancer cells in the peripheral blood of CRC patients. CONCLUSIONS: Using RT-PCR for the detection of CEA mRNA is feasible and may be a promising tool for early detection of micrometastatic circulating tumor cells in CRC patients. CRC patients expressing positive CEA mRNA in peripheral blood have a significantly higher risk of postoperative metastasis. Nevertheless, confirmation of CEA mRNA as a prognostic predictive factor requires the continuation of patient follow-up.
- ↑ Guadagni F, Detection of blood-borne cells in colorectal cancer patients by nested reverse transcription-polymerase chain reaction for carcinoembryonic antigen messenger RNA: longitudinal analyses and demonstration of its potential importance as an adjunct to multiple serum markers, Cancer res 2001 15 61(6) 2523, The use of reverse transcription-PCR (RT-PCR) to analyze cells in the blood of cancer patients for the detection of mRNA expressed in tumor cells has implications for both the prognosis and the monitoring of cancer patients for the efficacy of established or experimental therapies. Carcinoembryonic antigen (CEA) is expressed on approximately 95% of colorectal, gastric, and pancreatic tumors, and on the majority of breast, non-small cell lung, and head and neck carcinomas. CEA shed in serum is useful as a marker in only approximately 50% of colorectal cancer patients and rarely is shed by some other carcinoma types. RT-PCR has been used previously to detect CEA mRNA in cells in the blood and lymph nodes of cancer patients. Under the assay conditions validated in the studies reported here, 34 of 51 (67%) patients with different stages of colorectal cancer had blood cells that were positive by RT-PCR for CEA mRNA, whereas none of 18 patients with colonic polyps were positive; 2 of 60 apparently healthy individuals (who were age and sex matched with the carcinoma patients and were part of a colon cancer screening program as controls) were marginally positive. The results of CEA PCR in the blood of the carcinoma patients and the other groups showed strong statistical correlation with the disease (P2 < 0.0001). Analyses were carried out to detect both serum CEA protein levels and CEA mRNA in blood cells of colorectal carcinoma patients by RT-PCR. For all stages of disease, 18 of 51 patients (35%) were positive for serum CEA, whereas 35 of 51 (69%) were positive by RT-PCR. More importantly, only 5 of 23 (20%) of stage B and C colorectal cancer patients were positive for serum CEA, whereas 16 of 23 (70%) were positive by RT-PCR. The use of two other serum markers (CA19.9 and CA72-4) for colorectal cancer in combination with serum CEA scored two additional patients as positive; both were positive by RT-PCR for CEA mRNA. Pilot long-term longitudinal studies conducted before and after surgery identified some patients with CEA mRNA in blood cells that were negative for all serum markers, who eventually developed clinical metastatic disease. The studies reported here are the first to correlate RT-PCR results for CEA mRNA in blood cells with one or more serum markers for patients with different stages of colorectal cancer, and are the first long-term longitudinal studies to use RT-PCR to detect CEA mRNA in blood cells of cancer patients. Larger cohorts will be required in future studies to define the impact, if any, of this technology on prognosis and/or disease monitoring.
- ↑ Guller U, Disseminated single tumor cells as detected by real-time quantitative polymerase chain reaction represent a prognostic factor in patients undergoing surgery for colorectal cancer, Ann Surg 2002 dec 236(6) 768, OBJECTIVE: To evaluate the clinical relevance of real-time quantitative polymerase chain reaction (qPCR) detection of CEA and CK20 transcripts, as potentially related to tumor cell dissemination, in blood and peritoneal lavage from patients undergoing surgery for colorectal cancer. SUMMARY BACKGROUND DATA: Dissemination of single colorectal cancer cells in the peritoneal cavity, as well as in tumor drainage and peripheral blood vessels, might play a role in the metastasis process, thus affecting the clinical course. However, this phenomenon needs further elucidation. METHODS: In a prospective study the authors evaluated the potential of qPCR in the detection of CEA and/or CK20 transcripts in the peritoneal lavage fluid and in the peripheral and mesenteric venous blood of 39 patients undergoing curative resection for colorectal cancer. Peritoneal lavage and peripheral blood was sampled before and after tumor resection; mesenteric venous blood was sampled from the major tumor-draining vein immediately before clamping. After RNA extraction and reverse transcription, qPCR was performed using specific cDNA primers and probes for CEA and CK20. The dichotomous results from the qPCR were used as a predictor along with other covariates in Cox proportional hazard regression models of long-term outcome (disease-free survival and overall survival). RESULTS: Of 39 patients, 11 were positive. The median follow-up at analysis was 31 months for all patients. The dichotomous qPCR covariate was significant, with P =.001 and.0035 for disease-free survival and overall survival, respectively, in the proportional hazard regression models with only qPCR. In seven patients, disseminated colorectal cancer cells were found in the peritoneal lavage fluid but not in blood specimens; five of these patients (71%) had recurrence. CONCLUSIONS: These data suggest that detection of mRNA coding for CEA and/or CK20 using qPCR has potential clinical utility as a prognostic marker and should be evaluated in larger clinical studies. Identification of patients at high risk for metastatic disease after curative resection of colorectal cancer might be improved by analyzing peritoneal lavage specimens in addition to blood samples. This is based on the observation that in more than half of qPCR-positive patients, disseminated colorectal cancer cells were detected in peritoneal lavage specimens but not in blood samples, and that 71% of them had recurrence.
- ↑ Elshimali YI, The clinical significance of circulating tumor cells in the peripheral blood, Diagn Mol Pathol 2006 15(4) 187, Tumors launch malignant cells into the circulation continuously. In early stages, the immune surveillance system eliminates these cells from the circulation, but at later times they may persist longer and be detected. The first recorded evidence of the presence of circulating tumor cells in the peripheral blood of cancer patients was documented in 1869. Now, modern molecular biologic and cell sorting techniques make their detection and characterization more practicable. This review will consider the methods currently available for their detection and characterization, and the clinical implications of their presence in various malignant conditions.
- ↑ Mejean A, Detection of circulating prostate derived cells in patients with prostate adenocarcinoma is an independent risk factor for tumor recurrence, J Urol 2000 june 163 (6) 2022, PURPOSE: To determine whether the presence of prostate-derived cells in the peripheral blood circulation is a marker of prostate cancer and to define the clinical impact of the test. MATERIALS AND METHODS: We tested the peripheral blood of 99 patients with prostate adenocarcinoma (PAC), 79 of them undergoing radical prostatectomy, and 92 controls (31 healthy volunteers, 50 patients with adenoma and 11 with prostatitis) using a highly controlled procedure including reverse-transcriptase polymerase chain reaction (RT-PCR) targeted to prostate-specific antigen (PSA) mRNA. Patients were followed for 26 +/- 12 (range: 4 to 49) months. Forty tumor tissues were analyzed by immunohistochemistry for expression of p53 and E-cadherin antigens. RESULTS: Thirty three (33%) patients with PAC and 2 (2%) controls scored positive (p <0.0001) for the test. Detection of circulating prostatic cells was associated with development of metastases (p <0. 001), with relapse (p <0.001) and with a serum PSA level at diagnosis higher than 15 ng./ml. (p = 0.009). The rate of development of metastases according to time was significantly higher in patients who scored positive for the test (p <0.04). In a multivariate analysis, only the RT-PCR test was an independent risk factor associated with relapse (RR: 6.7). Finally, E-cadherin expression was significantly lower in the tumor tissues of positive patients as compared with those who scored negative for the test (p <0.01). CONCLUSIONS: This RT-PCR procedure, performed at diagnosis and with appropriate controls, is a clinically useful assay in evaluating the risk of tumor recurrence after radical prostatectomy in patients with PAC.
- ↑ Massimo Cristofanilli,Circulating Tumor Cells, Disease Progression, and Survival in Metastatic Breast Cancer, NEJM Vol 351 august 2004, http://content.nejm.org/cgi/content/abstract/351/8/78
- ↑ *http://www.istitutoncologicoveneto.it/it/rassegna/2012/201207-02.pdf (nature medicine No 20 december 2007
- ↑ Yoshihiro Hayata M.D, Significance of Carcinoma Cells in the Blood Relative to Surgery of Pulmonary Carcinoma, Chest 1964;46:51-60.) http://www.chestjournal.org/cgi/reprint/46/1/51
- ↑ Yamaguchi K, Ki-ras codon 12 point and P53 mutations: a molecular examination of the main tumor, liver, portal vein, peripheral arterial blood and para-aortic lymph node in pancreatic cancer, Am J Gastroenterol 2000 Aug 95(8), OBJECTIVE: Frequent P53 mutations and Ki-ras codon 12 point mutations have been reported in pancreatic cancer. Pancreatic cancer often recurs in the liver and/or lymph nodes shortly after a surgical resection. The purpose of this study is to elucidate the occurrence of microcirculating cancer cells and micrometastasis in pancreatic cancer. METHODS: P53 mutations and Ki-ras codon 12 point mutations were examined in the main tumor, liver, portal vein, and peripheral arterial blood, and para-aortic lymph nodes of patients with pancreatic cancer using molecular examinations. RESULTS: P53 mutations in the main tumor were present in nine (29%) of 31 patients with pancreatic cancer, whereas a Ki-ras codon 12 point mutation was evident in 18 (62%) of 29 examined patients. The peripheral arterial and portal vein blood and liver were positive for gene abnormalities in one (5%) of 21, in none (0%) of 19, and in one (1%) of 20, respectively. A P53 mutation in the main tumor was evident in none (0%) of seven stage I or II carcinomas and in nine (38%) of 24 stage III or IV cases, whereas a Ki-ras codon 12 point mutation was present in four (67%) of six stage I or II cases and in 14 (61%) of 23 stage III or IV cases. In addition, 15 (71%) of 21 patients with gene abnormalities (Ki-ras codon 12 point and/or p53 mutation) in the main tumor showed lymph node metastasis at surgery, whereas five (42%) of 12 without gene abnormalities did not demonstrate lymph node metastasis. Two (29%) of six patients with gene abnormalities in the main tumor and without metastatic disease at surgery developed liver metastasis within 6 months after surgery, whereas all five (100%) without the gene abnormalities and metastatic disease at surgery did not develop the metastasis, with the sensitivity being 100%, specificity 44%, the predictive value of the positive test 36%, and the predictive value of the negative test 100%. Two patients who had gene abnormalities in the para-aortic lymph node were free from histopathological metastasis and these two patients developed para-aortic lymph node metastasis within 6 months after surgery. CONCLUSIONS: A molecular examination of Ki-ras codon 12 and p53 mutations therefore enables us to predict, to some degree, the occurrence of liver and lymph node metastasis in pancreatic carcinoma.
- ↑ Georgakoudi I, In Vivo Flow Cytometry: A New Method for Enumerating Circulating Cancer Cells, Cancer Research 64, 5044-5047, August 1, 2004 http://cancerres.aacrjournals.org/cgi/content/full/64/15/5044
- ↑ Jaakkola S, Vornanen T, Leinonen J et al, Detection of prostatic cells in peripheral blood: correlation with serum concentrations of prostate specific antigen. Clin. Chem. 41:182-6,1995.
- ↑ Duffy M, Can molecular markers now be used for early diagnosis of malignancy?, Clin Chem 1995 Oct;41(10):1410-3 Most of the presently available cancer markers are neither specific for malignancy nor allow early diagnosis. However, the recent elucidation of the molecular events occurring during tumorigenesis may provide new markers that are likely to be both specific for cancer and sensitive for early disease. The key molecules undergoing alterations during carcinogenesis are the cellular oncogenes and suppressor genes. Alterations in these genes can be detected in cells shed from malignant and premalignant lesions. Thus, mutant p53 genes have been found in urine from patients with bladder cancer, mutant ras genes in stools from patients with colorectal and pancreatic cancers, and both mutant p53 and ras genes in sputum from patients with lung cancer. These findings show that the genetic alterations in cancer can be detected in fluids or secretions that had contact with the malignant tissue. The preliminary studies, however, had small numbers of both patients and controls and used time-consuming, labor-intensive, and expensive assays. For routine applications, these assays must be simplified, automated, and tested for sensitivity, specificity, and predictive value.
- ↑ Tarin D, Clinicopathological observations on metastasis in man studied in patients treated with peritoneovenous shunts, Br Med J 1984 march 10,288(6419) 749 Fourteen patients with inoperable cancer treated with peritoneovenous shunts for malignant ascites were studied post mortem. Clinical observations and findings at necropsy indicated that peritoneovenous shunting does not result in the establishment of clinically important haematogenous metastases and that metastases do not necessarily develop even when large numbers of viable tumour cells regularly enter the blood. Peritoneovenous shunting provides a unique opportunity for collecting data on the spread of tumours in man. http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1444638&blobtype=pdf
- ↑ Weiss L, Cell detachment and metastasis, Cancer Metastasis Rev 1983;2(2):111-27 Cancer cell detachment in three distinct and critical parts of the metastatic cascade is discussed. The detachment of cancer cells from their parent tumors is an initial early event in metastasis. The site of detachment with respect to proximity to blood vessels may determine the initial dissemination route. Many factors affect cell detachment; we specifically consider the effects of growth-rate, necrosis, enzyme activity, and stress on cell release in terms of metastasis-promoting mechanisms. Detachment is also discussed in relation to active cancer cell locomotion, where localized detachment from the substratum is a prerequisite for translatory movement. The importance of active cell movement in tissue invasion has only recently been assessed, and, in the case of at least some human malignant melanomas, a zone of actively moving cancer cells is believed to precede the growing body of the tumor. The secondary release of cancer cells from temporary arrest sites at the vascular endothelium consequent upon intravascular dissemination is also a major area of investigation. Circulating cancer cells arrest at vascular endothelium or are impacted in small vessels, however, most are released into the circulation and subsequently perish. The blood stream is a hostile environment, and it is probable that cancer cells are sufficiently damaged in translocation by hemodynamic trauma and humoral factors such that they easily detach or are 'sheared-off' the vascular endothelium by blood flow. Another possibility is that in some cases they are processed by 'first organ encounters' and perish before or shortly after arriving in a second organ. Animal studies have shown that, following intravenous injection, 60-100% of the injected dose of viable cancer cells are initially arrested in the lungs, but very few remain after 24 hr. As it is only those retained cells which produce tumors, the mechanisms involved in this secondary release, which occurs in all organs so far examined, are critical to any understanding of the metastatic cascade and metastatic inefficiency. The arrest of cancer cells at the vascular endothelium and their subsequent release have been associated with the presence of platelets, and the deposition of fibrin and manipulation of platelet-aggregating mechanisms and fibrinolysis are discussed in terms of their antimetastatic effects. The role of the reticuloendothelial system, natural killer cells, and polymorphs is discussed in relation to cancer cell clearance from blood vessels and also to inherent cancer cell properties which may act to inhibit their metastasis. Although detachment of cancer cells from a primary tumor may be regarded as metastasis promoting, secondary release of cancer cells may be associated with inhibition of metastasis.
- ↑ Nakamori S, Genetic detection of colorectal cancer cells in circulation and lymph nodes, Dis Colon Rectum 1997 40(10 sup) S29-36, PURPOSE: This study was undertaken to investigate the clinical implications of detection of genetic alterations in blood and lymph nodes in colorectal cancer patients. METHODS: The reverse transcriptase polymerase chain reaction product of the cytokeratin gene in blood was examined as a cancer cell-specific expression in 35 colorectal cancer patients. The K-ras or p53 gene mutations in the lymph nodes histopathologically negative for metastasis were studied by the mutant-allele-specific amplification method in 26 colorectal cancer patients. RESULTS: The reverse transcriptase polymerase chain reaction assay was able to detect a cytokeratin reverse transcriptase polymerase chain reaction product at a concentration from a single to ten colon cancer cells per 10(6) normal peripheral blood mononuclear cells. Cytokeratin reverse transcriptase polymerase chain reaction products were detected in nine patients' blood samples, although none of the samples were cytologically detectable. The blood's cytokeratin positivity correlated with the invasive mode of the tumor (P < 0.05) and the presence of distant metastasis (P < 0.01). Two (50 percent) of four patients whose blood was positive for cytokeratin had recurrences. Of 17 patients with the K-ras or p53 gene mutation in primary tumors, 9 (53 percent) had the corresponding mutations in lymph nodes. Mutation positivity in lymph nodes correlated with the presence of lymphatic invasion of the primary tumor (P < 0.05). All patients with mutation-negative lymph nodes remained disease-free for more than two years after surgery. CONCLUSION: Detection of cytokeratin reverse transcriptase polymerase chain reaction products in the blood and K-ras or p53 gene mutations in the lymph nodes histologically negative for metastasis may be applicable for clinical use, despite some limitations, and may serve as a useful clinical factor for stratifying patients who are at high or low risk for recurrence after surgery.
- ↑ Eriksson PS, Neurogenesis in the adult human hippocampus, nature med 1998 Nov;4(11):1313-7 The genesis of new cells, including neurons, in the adult human brain has not yet been demonstrated. This study was undertaken to investigate whether neurogenesis occurs in the adult human brain, in regions previously identified as neurogenic in adult rodents and monkeys. Human brain tissue was obtained postmortem from patients who had been treated with the thymidine analog, bromodeoxyuridine (BrdU), that labels DNA during the S phase. Using immunofluorescent labeling for BrdU and for one of the neuronal markers, NeuN, calbindin or neuron specific enolase (NSE), we demonstrate that new neurons, as defined by these markers, are generated from dividing progenitor cells in the dentate gyrus of adult humans. Our results further indicate that the human hippocampus retains its ability to generate neurons throughout life.
- ↑ McKay R, Stem cells in the central nervous system, Science 1997 Apr 4;276(5309):66-71, In the vertebrate central nervous system, multipotential cells have been identified in vitro and in vivo. Defined mitogens cause the proliferation of multipotential cells in vitro, the magnitude of which is sufficient to account for the number of cells in the brain. Factors that control the differentiation of fetal stem cells to neurons and glia have been defined in vitro, and multipotential cells with similar signaling logic can be cultured from the adult central nervous system. Transplanting cells to new sites emphasizes that neuroepithelial cells have the potential to integrate into many brain regions. These results focus attention on how information in external stimuli is translated into the number and types of differentiated cells in the brain. The development of therapies for the reconstruction of the diseased or injured brain will be guided by our understanding of the origin and stability of cell type in the central nervous system.
- ↑ Gage FH, Mammalian neural stem cells, Science 2000 Feb 25;287(5457):1433-8, Neural stem cells exist not only in the developing mammalian nervous system but also in the adult nervous system of all mammalian organisms, including humans. Neural stem cells can also be derived from more primitive embryonic stem cells. The location of the adult stem cells and the brain regions to which their progeny migrate in order to differentiate remain unresolved, although the number of viable locations is limited in the adult. The mechanisms that regulate endogenous stem cells are poorly understood. Potential uses of stem cells in repair include transplantation to repair missing cells and the activation of endogenous cells to provide "self-repair. " Before the full potential of neural stem cells can be realized, we need to learn what controls their proliferation, as well as the various pathways of differentiation available to their daughter cells.
- ↑ *http://www.ivis.org/docarchive/A1233.0405.pdf
- ↑ Von Holdt BM, The singular history of a canine transmissible tumor, Cell, 2006 Aug 11;126(3):445-7, In this issue of Cell, Murgia et al. (2006) confirm that the infectious agent of canine transmissible venereal tumor is the cancer cell itself and that the tumor is clonal in origin.
- ↑ Murgia C, Clonal origin and evolution of a transmissible cancer, Cell 2006 Aug 11;126(3):477-87, The transmissible agent causing canine transmissible venereal tumor (CTVT) is thought to be the tumor cell itself. To test this hypothesis, we analyzed genetic markers including major histocompatibility (MHC) genes, microsatellites, and mitochondrial DNA (mtDNA) in naturally occurring tumors and matched blood samples. In each case, the tumor is genetically distinct from its host. Moreover, tumors collected from 40 dogs in 5 continents are derived from a single neoplastic clone that has diverged into two subclades. Phylogenetic analyses indicate that CTVT most likely originated from a wolf or an East Asian breed of dog between 200 and 2500 years ago. Although CTVT is highly aneuploid, it has a remarkably stable genotype. During progressive growth, CTVT downmodulates MHC antigen expression. Our findings have implications for understanding genome instability in cancer, natural transplantation of allografts, and the capacity of a somatic cell to evolve into a transmissible parasite..
- ↑ *http://en.wikipedia.org/wiki/Devil_facial_tumour_disease
- ↑ *http://jvi.asm.org/cgi/content/abstract/73/8/6964
- ↑ Yutaka Tanaka, Experimental Cancer Cachexia Induced by Transplantable Colon 26 Adenocarcinoma in Mice, Cancer Research 50, 2290-2295, April 15, 1990 http://intl-cancerres.aacrjournals.org/cgi/content/abstract/50/8/2290, The present study investigates a tumor model for cachectic mice. Among various murine transplantable tumors, used for assessing cytostatics, we identified colon 26 adenocarcinoma (colon 26) as capable of causing cachexia. Fifteen days after inoculation, the tumor grew to about 6% of the body weight causing substantial carcass weight loss of 3.4 g (14.5% of the carcass weight). When the tumor size was 2.7 g at 3 weeks after the inoculation, the carcass weight was 12 g less than the age-matched control. The tumor continued to grow while the mice maintained this weight, surviving for an average of 45 days. This extensive weight loss was essentially the wasting of adipose and muscle tissues. Hypoglycemia and hypercorticism occurred during the time of the weight loss. In addition, the colon 26 caused disorders of hepatic functions: the concentration of acute phase proteins in serum increased; the number of hepatic glucocorticoid-cytosol receptors decreased; and activities of hepatic catalase and drug-metabolizing enzymes decreased. On the other hand, noncachectic mice with Meth A fibrosarcoma gained weight, which was somewhat less than the control, and had neither hypoglycemia nor hypercorticism, although some mild disorders of hepatic functions were found. Mice bearing colon 26 is an appropriate model for elucidating the mechanism that causes cachexia.
- ↑ [...] Interessant ist in dem Zusammenhang auch, daß bei eineiigen Zwillingen stets einer linkshändig und der andere rechtshändig ist [...] (from: http://www.neue-medizin.de/html/handigkeit.html)
- ↑ Hamer RG: Vermächtnis einer Neuen Medizin. Teil 2. Die 5 Biologischen Gesetze - Grundlage der gesamten Medizin.. 7. Aufl. Amici di Dirk - Ediciones de la Nueva Medicina S.L., E-Fuengirola 1999 ISBN 84-930091-0-5
- ↑ Derom, Handedness in twins according to zygosity and chorion type: a preliminary report Behav genet 1996 Jul;26(4):407
In the course of the East Flanders Prospective Twin Survey (EFPTS), handedness was assessed as part of a genealogical study (Meulemans et al., 1995) in 1616 twins (808 twin pairs) aged 6 to 28. Our findings are that, in this large population-based study with known placentation and zygosity, the often observed higher frequency of left-handedness in twins is confirmed, that it appears to be independent of zygosity and chorion type, and that the belief that discordant handedness in monozygotic twins represents mirror-imaging is mythical. - ↑ Shimizu A, Comparison of patterns of handedness between twins and singletons in Japan, Cortex 1983 Sep;19(3):345-52
The handedness questionnaire of thirteen items which was identical to that employed in our previous study on singletons was administered to 62 monozygotic (MZ) and 48 dizygotic (DZ) twin pairs in Japan. Information on forced conversion of hand usage in childhood was also obtained. Results indicated that the incidence of left-handedness was 3.6% and that of non-right-handedness (which includes mixed- and left-handedness) was 5.9%. There was no significant difference in the incidence of left-handedness or of non-right-handedness between MZ and DZ twin groups. The proportion of converted right-handedness in MZ twins was slightly higher than in DZ twins. MZ pairs were somewhat more concordant for handedness than DZ pairs. Item analysis indicated that the incidence of individuals who use the left hand for writing and eating was only 0.9% and 1.8%, respectively. A comparison of the results of the present survey on twins with those of our previous one on singletons revealed that the incidence of left-handedness or non-right-handedness in twins is the same as that in singletons. Twins (especially MZ twins) have experienced a forced conversion to right-hand usage more frequently than singletons. - ↑ Salk L, The effects of the normal heartbeat sound on the behavior of the new-born infant: implications for mental health. World Mental Health 1960 12, 168-175
- ↑ De Chateau, Left-side preference for holding and carrying newborn infants. Parental holding and carrying during the first week of life, J Nerv Ment Dis 1983 Apr;171(4):241-5,Four groups of adults were studied: new mothers, new fathers, fathers with older children, and males without children of their own. Nearly 80 per cent of all newly delivered mothers and fathers held their newborn infant against a point to the left of the body midline. Handedness and parity did not influence this preference, nor did the sex of the infant. The present study also demonstrates that new fathers during the neonatal period, as well as fathers with older infants, display a significantly greater preference for holding the infant to the left than males without own children and with or without experience of other children. Individual mother-father pairs held the infant on the same side of the body in the majority of couples studied. The pattern of infant-carrying showed no significant in-between group differences. The possible significance of these observations and their relation to other parental behavior are discussed.
- ↑ Mason Giorgia, Why do humans and apes cradle babies on their left side? New Scientist, 21. July 1990, 28.
- ↑ Sieratzki JS, Neuropsychological and neuropsychiatric perspectives on maternal cradling preferences, Epidemiol Psychiatr Soc 2002 Jul-Sep;11(3):170-6 OBJECTIVE: To assess competing explanations for the universal preference of mothers to cradle infants on their left side and to propose a relation to hemispheric asymmetry for social attachment and communication behaviour. METHODS: A review of observational, experimental, physiological, psychological, neuro-physiological, and neuro-psychological studies, including new findings on the cradling behaviour of mothers with auditory or visual impairments. RESULTS: A significant left-cradling bias is observed in both right- and left-handed mothers which cannot adequately be explained by arguments based on handedness or closer contact to the soothing sound of the maternal heartbeat. Observations of primate behaviour have led to the suggestion that the left-cradling bias may be related to a left visual field (right hemisphere) advantage for monitoring an infant's facial expressions of distress. However, more than just monitoring, cradling subserves the mother's connection with the infant. For that reason, we have suggested that left cradling might be related to a right hemisphere specialisation for emotional communication, i.e. the speech melody, smiles, signals, and stroking which mothers use to interact with their infants. Studies of mother-infant interaction show that the sound of the mother's voice is more soothing when cradling on the left, more stimulating when cradling on the right. Cradling laterality may thus be related to emotional state and behavioural intent. There is also evidence to suggest that left cradling is linked to a special role of the right hemisphere in social attachment behaviour. This function may be disturbed in mothers with post-natal depression who show abnormal right hemisphere activity. CONCLUSION: Cradling embodies the symbiotic relationship between mother and infant; various lines of evidence support the suggestion that the universal preference of mothers to cradle infants on their left side is related to a right hemisphere dominance for social attachment and communication behaviour.
- ↑ Bogren LY, Side preference in women and men when holding their newborn child: psychological background, Acta Psychiatr Scand 1984 Jan;69(1):13-23 In a prospective study 81 randomly selected parents awaiting their first baby were interviewed early during pregnancy and again during the week after delivery. About 80% of the women and their partners were found to hold their child to the left, and 20% to the right, irrespective of handedness. There was no relation between side preference in child holding in the couples. Common to both sexes is the trend that left-holders are more attached to and identified with the parent of their own sex whereas right-holders are more attached to and identified with the parent of the opposite sex. Right-holders have also more often had mental symptoms prior to pregnancy and were concerned about the pregnancy, delivery and health of the child at birth.
- ↑ Bogren LY, The couvade syndrome and side preference in child holding, Acta Psychiatr Scand 1985 Mar;71(3):311-4,In a prospective study of expectant couples 20% of the men suffered from the couvade syndrome. About 80% of both women and men hold their newborn infant to the left and 20% to the right, irrespective of handedness. Compared with others, men with the syndrome more frequently developed a right-side preference in child holding. Right-holding men more often had sons than daughters. Right-holders with the couvade syndrome were more often attached to and more closely identified with their mothers than were right-holding non-sufferers.
- ↑ Ginsburg HJ, Maternal holding preferences: a consequence of newborn head-turning response, Child Dev 1979 Mar;50(1):280-1, Salk observed that in an overwhelming majority of cases (80%) mothers prefer to hold their infants across the left shoulder. This preference occurs over a diversity of cultures and is not related to the hand preference of the mother. Salk suggested a fetal imprinting to the sound of the heartbeat as the mechanism responsible for this phenomenon. While such speculation is intriguing, it is not scientifically testable. 2 experiments were performed to examine a more testable hypothesis. Results of these studies suggest that the initial head-turning preference of an infant is related to the holding preference of its mother.
- ↑ Weiland JH, Patterns of mother-infant contact: the significance of lateral preference, J Genet Psychol 1970 117 157
- ↑ Souza-Godeli MR, Lateral cradling preferences in children, Percept Mot Skills 1996 Dec;83(3 Pt 2):1421-2 Lateral preferences for cradling a doll and for holding a package were investigated among children from 2- to 6-yr-old. Results showed a preference for holding a baby on the left side of the body in children as young as 3 yr. old. The data favour the hypothesis of an early emergence of this pattern of behavior in the human ontogenesis.
- ↑ Lucas MD, Laterality of cradling in relation to perception and expression of facial affect, J Genet Psychol 1993 Sep;154(3):347-52. A dominant leftward cradling bias has been observed in women in non feeding interaction with infants. Reasons for this behavior have been sought in behavioral asymmetries, but none have sufficiently justified the presence of this leftward pattern. Recently, the cradling bias has been linked to affective processing, considered to be a specialized function of the nondominant (right) hemisphere (Manning & Chamberlain, 1990). This study investigates Manning and Chamberlain's (1990) suggestions that a relationship exists between leftward cradling and the interpretation and expression of affect. Eighty-six nulliparous women were tested for this relationship by correlating direction of cradling bias with visual field dominance for perception of facially expressed emotion and expression of affect. No significant relationship was found to directly support the hypotheses.
- ↑ Harris LJ, Side preference in adults for holding infants: contributions of sex and handedness in a test of imagination, Brain Cogn 2000 Jun-Aug;43(1-3):246-52, Five hundred one right-handers (150 men, 351 women) and 53 left-handers (15 men, 38 women) were asked to imagine holding a young infant in their arms. Right-handers reported significant left-side biases--in 68% of the men and 73% of the women. For left-handers, side preferences were weaker, the left-side bias dropping to 47% for men and 60% for women, with neither figure different from chance. The results are discussed in the context of theory and research on the functional neuroanatomy of attention, emotional arousal, and the generation, maintenance, and manipulation of mental images.
- ↑ Harris LJ, Lateral biases for holding infants: early opinions, observations, and explanations, with some possible lessons for theory and research today, Brain Cogn 2002 Mar-Apr;48(2-3):392-4, In 1962, the psychologist Lee Salk reported finding that 80% of mothers held their infants on the left side of their body, so that the infant's head was to their left. Salk's finding has been amply confirmed, with new studies of mothers as well as other adults reporting figures for left-side holding ranging from 60 to 85% (e.g., de Chateau, 1983; Harris & Fitzgerald, 1985; Harris, Almerigi, & Kirsch, 2000). New studies also suggest that the bias is only for holding infants (or infant dolls), not for books, packages, or other objects (e.g., Almerigi, Carbary, & Harris, 2001; Rheingold & Keene, 1965). The possibility that it is unique to infants (or their likenesses) is what gives it special interest for investigators who study laterality of function. The discovery of the bias is often credited to Salk, but it would be more accurate to say that he rediscovered it because it was first noted at least two hundred years earlier, then, evidently, forgotten, only to be rediscovered and again forgotten several times through the early decades of the twentieth century. Over this period, however, not all agreed that the preferred side was the left: a nearly equal number said it was the right. Each group also proposed explanations for why one or the other side was preferred. They also foresaw different consequences for the infant being held. In the 1980s, I briefly described some of the early reports in essays on the history of theories and research on laterality of function (Harris, 1980, 1983). A manuscript now in preparation provides a more comprehensive description and evaluation of these reports and suggests certain lessons they may hold for current theory and research. The poster proposed for TENNET XII will summarize the main points of this new review and analysis. The poster will be organized into 6 sections, with bulleted text accompanied by drawings, photographs, and other illustrations. The plan is to make the story as visual as possible.
- ↑ http://www.sussex.ac.uk/press_office/bulletin/13feb04/article1.shtml
- ↑ Reissland N 2000 http://www.abdn.ac.uk/~psy215/dept/cradling%20bias%20in%20relation%20to%20child%20directed%20language%202000.pdf
- ↑ Hardyk C Petrinovich LF, Left-handedness, Psycol Bull, 1977 May; 84(3):385-404
- ↑ Perelle IB Ehrmann L, An international study of human handedness: the data, Behv Genet, 1994 May;24(3):217-27, Human handedness has been the subject of systematic study since 1646, but there is no agreement among researchers as to who can be considered a left-hander, what is the etiology of left-handedness, or what the proportion of left-handedness is in the world's population. This article reports the results of a handedness survey administered to 12,000 subjects in 17 countries, the largest handedness survey attempted. The paper discusses methods for determining handedness, the probability of a genetic component for handedness, and the relationship of sex, birth order, multiple birth, and first-degree relative's handedness on subject's handedness. A hypothesis for the etiology of left-handedness is presented.
- ↑ Raymond M, Frequency-dependent maintenance of left handedness in humans, Proc Biol Sci, 1996 Dec 22;263(1377):1627-33, The percentage (10-13%) of left handedness in human has apparently not changed since the Neolithic. Left handedness is heritable and appears to be repeatedly associated with some reduced fitness components; the persistence of left handedness implies that left handers have a fitness advantage in some situations. We propose that left handers have a frequency-dependent advantage in fights and for that reason a fitness advantage. To test this hypothesis, left handedness frequencies in the general population and in sporting individuals (both students and the sporting elite) have been compared, as sporting performance is likely to be a good indicator of fighting abilities. The higher proportion of left-handed individuals in interactive sports (reflecting some fighting elements), reaching 50% in some sports categories, but not in noninteractive sports, is consistent with the fighting hypothesis. The greater frequency of left handedness in males than in females is also consistent with this hypothesis, as male-male fights are universally more frequent than other combinations. The frequency-dependent advantage in fights of left handers might explain the stability of left handedness.
- ↑ Medland SE, Special twin environments, genetic influences and their effects on the handedness of twins and their siblings, Twin Res 2003 Apr;6(2):119-30, It has been suggested that twinning may influence handedness through the effects of birth order, intra-uterine crowding and mirror imaging. The influence of these effects on handedness (for writing and throwing) was examined in 3657 Monozygotic (MZ) and 3762 Dizygotic (DZ) twin pairs (born 1893-1992). Maximum likelihood analyses revealed no effects of birth order on the incidence of left-handedness. Twins were no more likely to be left-handed than their singleton siblings (n = 1757), and there were no differences between the DZ co-twin and sibling-twin covariances, suggesting that neither intra-uterine crowding nor the experience of being a twin affects handedness. There was no evidence of mirror imaging; the co-twin correlations of monochorionic and dichorionic MZ twins did not differ. Univariate genetic analyses revealed common environmental factors to be the most parsimonious explanation of familial aggregation for the writing-hand measure, while additive genetic influences provided a better interpretation of the throwing hand data.
- ↑ Searleman A,Laterality in twins: the relationship between handedness and hemispheric asymmetry for speech, Behav Genet. 1978 Jul;8(4):349
- ↑ Reiss M, Laterality in twins,Z. Morphol Anthropol. 1996 Sep;81(2):14, The literature on twins and laterality is reviewed: Both monozygotic (MZ) and dizygotic twins (DZ) show a low concordance in all functional and morphological asymmetries. The proportions of R-R, R-L and L-L pairs in MZ twins and in DZ twins are in binomial distribution. The incidence of left-handedness is the same in MZ twins and DZ twins, but higher than in singletons. Other laterality signs do not show this tendency. The whole issue of twinning is as yet unresolved, yet it is clear already that no simple genetic model for the inheritance can be applied. The present review discusses three genetic models and associated problems with each. The overall tendency to a higher rate of left-handedness in twins could be due to such pathological factors (associated with twinning) as intrauterine crowding and perinatal stress, but is not due to so-called "mirror imaging"-phenomena in twins.
- ↑ Derom, Handedness in twins according to zygosity and chorion type: a preliminary report Behav genet 1996 Jul;26(4):407 In the course of the East Flanders Prospective Twin Survey (EFPTS), handedness was assessed as part of a genealogical study (Meulemans et al., 1995) in 1616 twins (808 twin pairs) aged 6 to 28. Our findings are that, in this large population-based study with known placentation and zygosity, the often observed higher frequency of left-handedness in twins is confirmed, that it appears to be independent of zygosity and chorion type, and that the belief that discordant handedness in monozygotic twins represents mirror-imaging is mythical.
- ↑ Coren S Porac C, Fifty centuries of right-handedness: the historical record, Science 1977 Nov 11;198(4317):631-2 A survey of more than 5000 years of art work, encompassing 1180 scorable instances of unimanual tool or weapon usage, revealed no systematic trends in hand usage. The right hand was used in an average of 93 percent of the cases, regardless of which historical era or geographic region was assessed.
- ↑ Peter Hepper, Signaling right from the womb, Belfast 2004 New Scientist 2457, pag 13, 24 July 2004 [2]
- ↑ Swiss Study Group for Complementary and Alternative Methods in Cancer, SCAC. Hamer's «New Medicine» Document No. 01/02. [3]
- ↑ http://www.thescientificworldjournal.com/headeradmin/upload/2005.03.16.pdf
- ↑ Vermächtnis einer Neuen Medizin
- ↑ http://www.promed-ev.de/modules/news/article.php?storyid=105